Scientists Discover How Cells Hit a Tipping Point and Turn Healthy Tissues into Diseased Ones
A new study from Washington University in St. Louis and Tsinghua University in Beijing has uncovered how cells in tissues can suddenly switch from a healthy, disordered state to a coordinated, disease-driving state. This finding provides one of the clearest explanations yet for why fibrotic diseases—conditions involving excessive tissue scarring in organs like the lungs, liver, kidneys, and heart—tend to progress in sudden, dramatic bursts instead of gradually.
The study, published on October 3, 2025, in the Proceedings of the National Academy of Sciences (PNAS), describes this phenomenon as a kind of biological phase transition, similar to how water freezes into ice or metal becomes magnetic at a specific temperature. The researchers found that tissues can undergo a comparable transformation when cells reach a critical distance that allows them to start communicating mechanically through their surrounding collagen network.
The Discovery: When Cells Start Talking Through the Matrix
Cells in the body constantly interact with their environment by pulling and pushing against it. These mechanical forces are crucial for normal physiological processes—bones strengthen with exercise, wounds close after injury, and tissues maintain their structure.
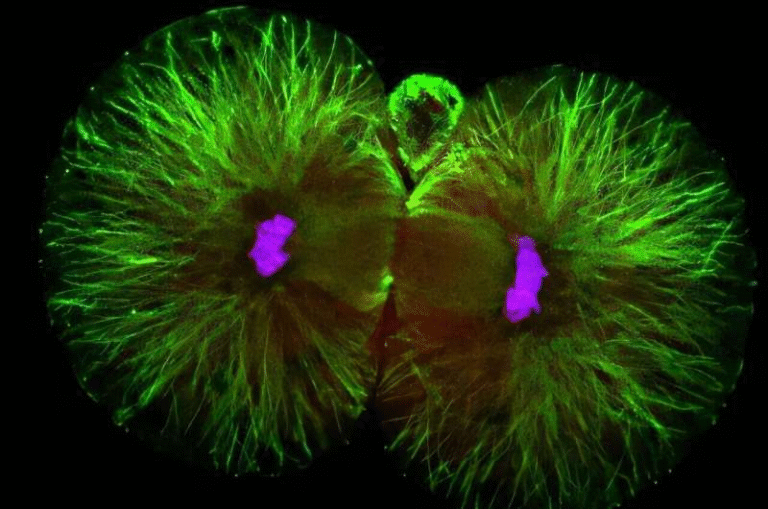
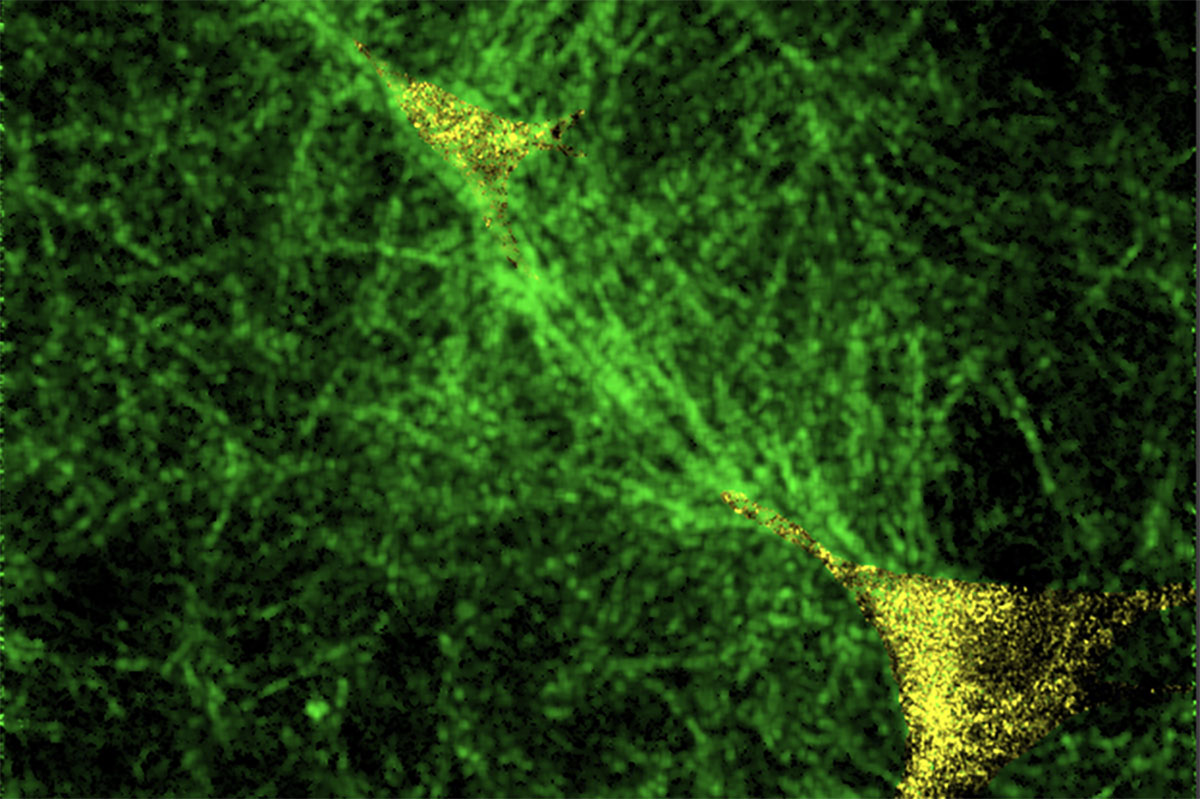
But this new research reveals that when cells get close enough to each other, they can begin to communicate mechanically through the fibrous collagen that surrounds them. These collagen fibers become aligned and form stiff “tension bands”—essentially microscopic highways that transmit mechanical signals between nearby cells.
When enough of these bands form, the entire tissue can abruptly shift from a disordered, independent state to a coordinated, collective state. In this collective state, cells behave in sync, often amplifying processes like fibrosis, which is the body’s overzealous attempt to repair tissue but ends up scarring it instead.
If cells are too far apart, they can’t form these tension bands and remain mechanically isolated, even if they’re in the same tissue. That’s why fibrosis doesn’t creep up gradually—it snaps into place once this communication threshold is crossed.
The Critical Distance and the “Mechanical Tipping Point”
Through computational modeling, the team pinpointed what they call the mechanical tipping point—a critical spacing between cells where this sudden coordination begins.
When cells are separated by more than a few hundred micrometers, they act independently. But once the distance drops below that threshold, they start influencing each other’s behavior mechanically. This transition is sharp and sudden, not gradual.
The exact point depends on how the collagen fibers in the extracellular matrix (ECM) deform under stress. The ECM is a 3D web of proteins, mainly collagen, that provides structural support to tissues. Its fibers can bend, stretch, and align depending on the forces applied by cells.
Why Collagen Fiber Behavior Matters
The researchers showed that this phase transition happens because fibrous materials like collagen can carry mechanical signals over long distances—unlike uniform materials such as rubber.
If cells were embedded in something like rubber, they wouldn’t be able to feel their neighbors’ forces even at close range. But in a fibrous network, once collagen fibers are stretched beyond a certain point, they align and stiffen, allowing forces to travel much farther.
This property is defined by the critical stretch ratio—the amount of stretch needed before fibers line up. That stretch ratio depends on collagen crosslinking, which increases naturally with aging, and is also influenced by diet, blood sugar levels, and metabolic diseases such as diabetes.
In short, the stiffer and more crosslinked the collagen becomes, the more easily these mechanical pathways can form. But at the same time, too much crosslinking can reduce how far signals travel, creating a delicate balance.
Why Fibrosis Progresses in Bursts
Fibrosis involves an overproduction and hardening of collagen in tissues. It’s a hallmark of chronic diseases in organs like the liver (cirrhosis), lungs (pulmonary fibrosis), and heart (cardiac fibrosis).
The study reveals a key paradox: as tissues become more crosslinked with age or disease, the cells become more contractile—that is, they pull harder on their surroundings. But this same crosslinking also shortens the distance that mechanical signals can travel.
In early fibrosis, moderately activated cells can still communicate over long distances, allowing the disease to spread across tissue. Later on, as crosslinking increases, communication becomes more localized—but by that time, the cells have already multiplied, and their spacing has dropped below the critical threshold. The system has effectively tipped over into coordinated scarring.
Why Many Fibrosis Treatments Fail
Many current anti-fibrotic therapies focus on reducing tissue stiffness—essentially trying to “soften” the fibrotic tissue. But this study shows that this strategy might not address the root of the problem.
Simply softening tissue doesn’t necessarily stop cells from coordinating. The key lies in breaking the communication network itself—either by keeping cells from getting close enough, or by altering the fiber properties that let tension bands form.
This insight may explain why so many clinical trials targeting stiffness alone have struggled to deliver major breakthroughs. The real challenge might be disrupting mechanical communication, not just altering stiffness levels.
New Therapeutic Ideas
The study points to several potential intervention strategies. These include reducing collagen crosslinking, blocking fiber alignment, or using biomaterials that interfere with long-range mechanical signaling.
It also hints that dietary changes could play a role. Since collagen crosslinking is affected by advanced glycation end products—molecules that form when sugar binds to proteins—reducing these through dietary means might help slow down or prevent tissues from reaching the tipping point.
In other words, what we eat could subtly influence how our tissues communicate mechanically over time.
Aging, Crosslinking, and the Inevitable Drift Toward Disease
The findings also shed light on why fibrotic diseases become more common with age. Over time, collagen fibers naturally accumulate crosslinks, even in healthy individuals. This makes tissues stiffer and more brittle, and shifts their properties closer to the critical threshold where small triggers—like an injury or infection—can set off fibrosis.
Think of it as a ticking clock inside your tissues. As years pass, the collagen network slowly approaches a point of instability. Then, one day, an ordinary wound or mild inflammation might be enough to push the system past its tipping point, leading to runaway scarring.
The Bigger Picture: Mechanobiology and the Physics of Life
This study adds to a growing field called mechanobiology, which explores how physical forces shape biological behavior. For decades, researchers have focused mainly on biochemical signals—hormones, enzymes, genes—but it’s becoming clear that mechanical cues are just as powerful.
The concept of a phase transition in tissue behavior is a fascinating bridge between physics and biology. Just as molecules can collectively freeze, magnetize, or superconduct, cells too can exhibit collective physical behavior once the right conditions are met.
It suggests that living tissues obey the same universal principles of organization and order that govern non-living systems—a reminder that biology, at its core, is still subject to the laws of physics.
Why This Matters for the Future
Understanding these mechanical tipping points could change how we approach chronic diseases. Instead of fighting the biochemical aftermath—like inflammation or scarring—we might one day tune the mechanical environment of tissues to prevent those diseases from starting in the first place.
That could mean designing smarter biomaterials for implants, new drugs that tweak fiber alignment, or even lifestyle interventions that slow collagen crosslinking through diet and exercise.
As the study’s researchers put it, this is not about fighting against the body’s mechanical systems, but working with them. If we can learn to control these phase transitions, we might finally find ways to stop fibrosis before it starts.
Research Paper: Fiber recruitment drives a phase transition of cell polarization at a critical cell spacing in matrix-mediated tissue remodeling (PNAS, 2025)