Personalized Prehabilitation Before Major Surgery Shows Strong Benefits for Immunity, Fitness, and Recovery

Major surgery is a stressful event for both the body and the mind, and doctors have long encouraged patients to eat better, stay active, reduce stress, and get quality sleep in the weeks leading up to an operation. This preparation period is known as prehabilitation, or prehab. While the idea isn’t new, many patients struggle to follow these recommendations consistently. A new randomized clinical trial from Stanford Medicine offers strong evidence that adding personalized coaching to prehab can significantly improve patient resilience, immune readiness, and post-surgical outcomes.
This study, published in JAMA Surgery, compared traditional prehab—usually delivered through written guidelines—to a more hands-on approach that includes twice-weekly one-on-one coaching. Researchers found that personalized coaching produced measurable improvements across the board: better physical performance, stronger cognitive scores, reduced markers of immune over-reactivity, and fewer moderate-to-severe complications after surgery. The findings suggest that personalized prehab may act almost like “training” for the body before a major physical challenge.
What the Study Measured
Researchers enrolled 58 adult patients at Stanford Health Care between June 2020 and September 2022, all of whom were scheduled for major elective surgeries. These surgeries included abdominal, thoracic, neurosurgical, and plastic/reconstructive operations. After applying exclusion criteria—such as unsafe exercise limitations, very high anesthesia risk, palliative care status, or having less than two weeks between enrollment and surgery—54 patients completed the trial.
Participants were randomly assigned to one of two groups:
- Standard Prehab Group (27 patients)
– Received a paper booklet with guidance on exercise, nutrition, mindfulness, and cognitive training.
– Content included structured strength and cardio routines, a Mediterranean-style dietary outline, a simple mindfulness method, and access to a brain-training app. - Personalized Prehab Group (27 patients)
– Received the exact same core content areas, but with twice-weekly individualized coaching via remote video calls.
– One session each week focused on exercise, led by a physical therapist.
– The other session focused on nutrition, cognitive habits, and behavioral guidance, led by a physician.
– Everything was tailored to each patient’s abilities and actual lifestyle. For example, nutrition plans were based on real photos and videos of a patient’s kitchen, groceries, or typical meals.
The aim was not only to compare physical and cognitive improvements, but also to examine differences in immune system behavior—which plays a central role in controlling infections, healing wounds, and recovering strength after surgery.
Prehab as “Training” for the Body
Major surgery creates a surge of biological stress, similar in scale to running a marathon or undergoing a major physical trauma. Physicians have long argued that patients should prepare for this event similarly to how athletes train before a contest. But without support, many patients don’t follow through effectively.
The Stanford team wanted to identify whether personalization—actual human coaching—would improve patient adherence and create meaningful, measurable improvements before surgery. They also wanted to understand why prehab works on a biological level, particularly when it comes to the immune system.
Physical and Cognitive Improvements
Before starting the prehab program, all patients completed a series of physical and cognitive tests and repeated them right before surgery. Results showed a major difference between groups:
- The personalized prehab group improved significantly on every physical and cognitive test.
- The standard group improved only in walking distance, with no meaningful gains in other areas.
In one example, the personalized group showed a median increase in their 6-Minute Walk Test, rising from around 496 meters to 546 meters. This type of improvement reflects better endurance, mobility, and cardiopulmonary readiness—all important factors during post-operative recovery.
Immune System Modulation
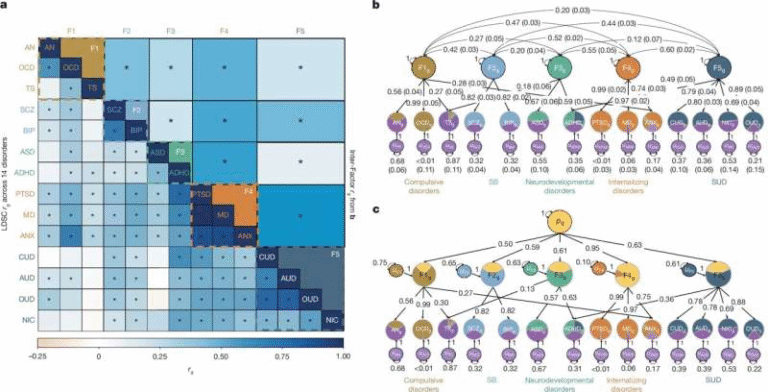
One of the most important contributions of this study is its deep look at immune system changes. Using a 47-marker mass cytometry panel, researchers analyzed how different types of immune cells responded to laboratory stimulation mimicking conditions present during surgery.
They found:
- The personalized group showed significantly reduced over-reactivity in certain innate immune cells, including classical monocytes and myeloid-derived suppressor cells.
- These cells displayed lower activation of the powerful pro-inflammatory pathway phosphorylated ERK1/2 after stimulation with cytokines like IL-2, IL-4, and IL-6.
- Adaptive immune cells (particularly Th1 cells) showed reduced activation in the phosphorylated CREB pathway.
- Patients also demonstrated lower baseline inflammation leading up to surgery.
Researchers note that individuals who develop infections after surgery often show abnormally high innate immune activity before the operation. By reducing this over-reactivity, personalized prehab may lower the risk of post-surgical infections and other complications.
A statistical analysis confirmed how distinct the immune changes were:
- Personalized prehab produced a clear shift in immune profiles (AUROC 0.88), meaning a strong separation between pre- and post-prehab immune activity.
- Standard prehab produced no meaningful change (AUROC 0.63).
These findings are especially impressive because this level of immune modulation is typically associated with pharmacological treatments, not simple lifestyle adjustments done at home.
Reduction in Post-Surgery Complications
The most important real-world outcome: fewer complications.
Within 30 days after surgery:
- 11 of 27 patients in the standard group experienced moderate-to-severe complications (Clavien-Dindo grade > 1).
- Only 4 of 27 patients in the personalized group experienced complications of similar severity.
This difference was statistically significant and supports the idea that personalized prehab can help patients not only prepare better, but also recover better.
Why Personalized Coaching Works
Participants expressed that they preferred the personalized approach because:
- It offered real human connection during a stressful time.
- Remote sessions made it easier to stay consistent.
- Tailoring made the program feel achievable.
- They appreciated having experts who monitored their progress and guided them.
Because of this, adherence to the personalized program was much higher. When patients actually follow prehab recommendations, the results naturally become more meaningful.
Broader Context: What We Know About Prehab
Research over the past decade has shown that prehab can help with:
- Improving respiratory function
- Reducing hospital stays
- Enhancing mental readiness
- Lowering surgical risks for older adults
- Improving overall functional recovery
However, many earlier studies suffered from inconsistent methods, low personalization, or unclear biological mechanisms. This new Stanford study stands out because it connects specific immune changes with actual clinical outcomes, helping establish a clearer scientific foundation for prehab.
Still, the trial size was small, and researchers agree that larger studies are needed to confirm the findings and refine which patients benefit the most.
A Simple Takeaway for Patients Preparing for Surgery
While personalized prehab may not yet be widely available, anyone preparing for major surgery can take small steps:
- Focus on regular exercise, even walking.
- Improve nutrition, especially whole foods and lean proteins.
- Prioritize sleep quality.
- Practice simple stress-management habits.
- Stay mentally active with light cognitive exercises.
Researchers emphasize that even a single small habit can create momentum. Prehab can empower patients at a moment when they often feel helpless—and can turn anxiety into preparation.
Research Paper Link:
https://jamanetwork.com/journals/jamasurgery/fullarticle/2841299