Plant-Based Diet Shows Strong Potential to Prevent and Reverse a Form of Heart Disease Linked to Hypertension
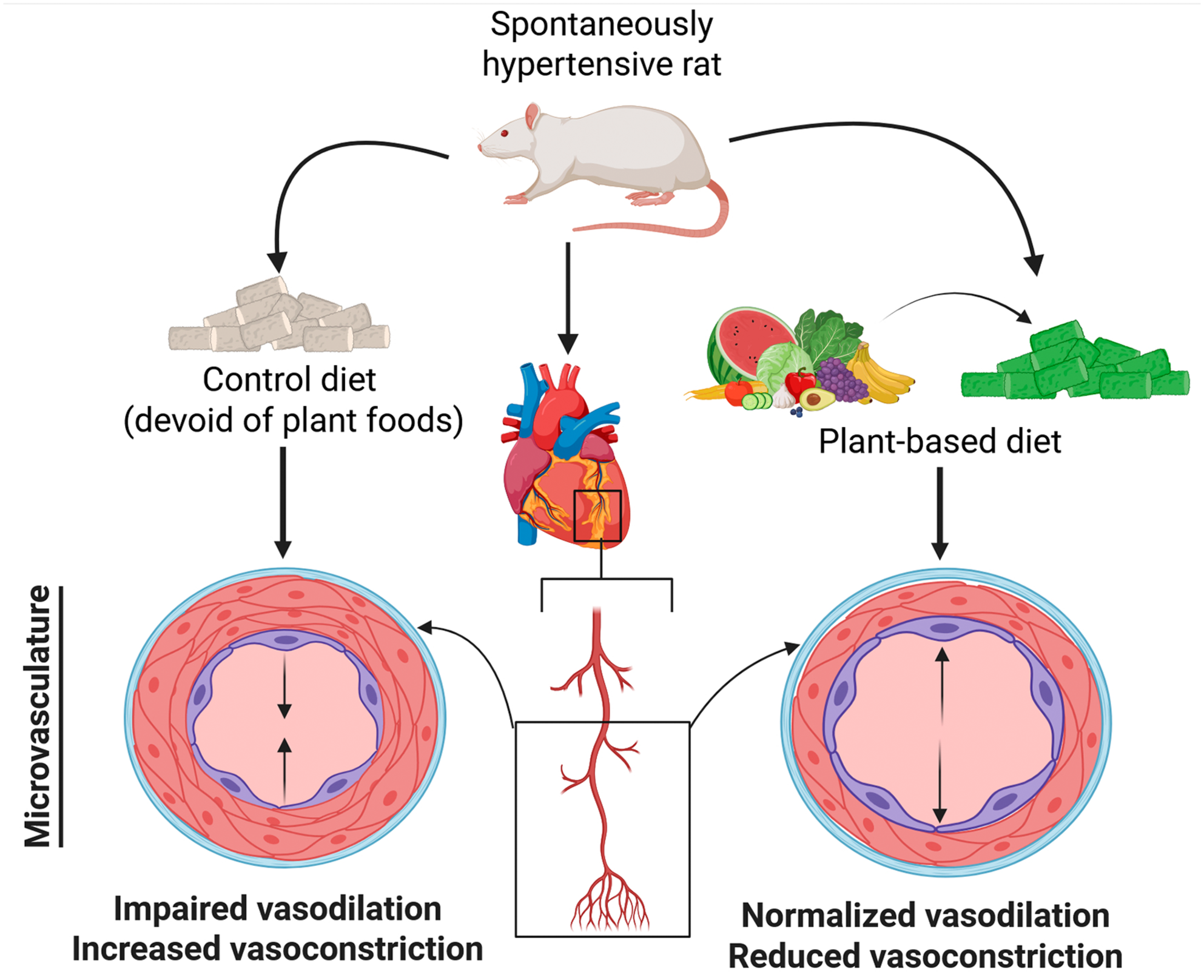
A new study from researchers at Georgia State University has uncovered a compelling connection between diet and heart health in animals with high blood pressure. The findings suggest that a plant-based diet, rich in fruits, vegetables, nuts, and legumes, can both prevent and reverse a damaging heart condition known as coronary microvascular dysfunction (CMD). This type of heart disease affects the tiny blood vessels responsible for delivering blood to the heart muscle and is notoriously difficult to treat. The study stands out because it demonstrates a significant improvement in heart microvascular function even when hypertension remains present, meaning the diet provided benefits independent of lowering blood pressure.
Below is a detailed breakdown of the study, its methods, its surprising results, and extra information that helps make sense of why these findings matter.
Understanding Coronary Microvascular Dysfunction (CMD)
CMD is a disorder that develops when the small coronary blood vessels fail to properly dilate or regulate blood flow. Unlike classic coronary artery disease, CMD does not involve major arterial blockages, which makes it harder to detect and often harder to treat.
This condition is a major contributor to chest pain, hospitalizations, heart failure, and in some cases even sudden cardiac events. A particularly notable fact is that CMD affects women more frequently and more severely than men, with women showing higher hospitalization rates after diagnosis.
Because current therapeutic strategies deliver only moderate results, researchers have been searching for new, non-pharmaceutical approaches to improve microvascular function. This study is one of the first to directly look at how dietary patterns influence CMD progression.
What the Study Did
Researchers used female spontaneously hypertensive rats, a well-established model for studying high blood pressure and cardiac complications. The experiment ran for six months and included two primary groups:
- Rats fed a refined, nutrient-matched control diet lacking plant foods.
- Rats fed a plant-based diet containing 28% fruits, vegetables, nuts, and legumes.
Importantly, both diets were carefully matched for calories, fat, protein, carbohydrates, and micronutrients. This deliberate matching means that the only meaningful difference between the diets was the high antioxidant content and naturally occurring bioactive compounds from plant-based ingredients.
After six months, researchers introduced a third group: rats that had been on the control diet but were then switched to the plant-based diet to see if already established CMD could be reversed.
What the Human Equivalent of the Diet Looks Like
To help translate the dietary intervention into human terms, the researchers provided a detailed daily breakdown. A person eating the equivalent diet would consume:
- One cup of black beans
- One large red bell pepper
- 1½ cups of Brussels sprouts
- Two lemons
- One medium sweet potato
- 1½ cups of walnuts
- One cup of blueberries
The emphasis here is on whole plant foods, which offer a combination of antioxidants, fiber, polyphenols, vitamins, and minerals.
How the Researchers Measured CMD and Heart Function
The team used several advanced techniques to examine the condition of the rats’ hearts:
- Coronary Flow Reserve (CFR): A clinically relevant measurement that assesses how well coronary vessels increase blood flow under stress.
- Cardiac Magnetic Resonance Imaging (MRI): Performed using Georgia State University’s Advanced Translational Imaging Facility to visualize blood flow in heart muscle.
- Cellular Functional Tests: Blood vessel cells were isolated from the animals’ hearts to examine how well they functioned in response to normal biological signals.
- Tissue Analysis: Heart tissue was examined for inflammation, oxidative damage, and markers of cellular stress.
These combined methods allowed the team to evaluate CMD from whole-organ blood flow down to cellular behavior.
Key Findings of the Study
The outcomes were not only promising, but in some ways unexpected:
1. The Plant-Based Diet Prevented CMD
Animals genetically predisposed to hypertension but given the plant-based diet did not develop CMD, even after six months of chronic high blood pressure.
2. The Diet Also Reversed Existing CMD
Rats that already had CMD but were switched to the plant-based diet showed a restoration of healthy coronary microvascular function.
3. The Benefits Occurred Despite Persistent Hypertension
This was one of the most striking results. The animals remained hypertensive, yet their microvascular function still improved. This suggests the diet exerted a direct protective effect on the small coronary vessels, separate from blood pressure regulation.
4. Improved Cellular Function
Damage to endothelial cells often leads to constricted vessels and poor blood flow. The plant-based diet restored proper functioning of these cells, allowing blood vessels to dilate normally again.
5. Reduced Tissue Damage
Markers of oxidative stress, inflammation, and fibrosis were significantly lower in rats that consumed the plant-based diet.
Collectively, these effects show that a whole-food plant-based diet may offer a powerful and targeted way to protect heart microvasculature.
Why These Findings Matter
CMD is difficult to diagnose and even harder to treat. Many patients with persistent chest pain are found to have no major arterial blockages, yet they continue to experience symptoms due to impaired microvascular function. Because existing drugs offer limited benefits, the possibility of using a dietary approach opens a new avenue for treatment.
Another major implication is that these benefits occurred independent of blood pressure control. Many people struggle to bring their hypertension down despite medication and lifestyle changes. A therapy that can protect the heart even when high blood pressure persists could be transformative.
Finally, since CMD disproportionately affects women, a non-invasive and accessible way to reduce symptoms and improve vessel function could help an underserved patient population.
Additional Information About Plant-Based Diets and Heart Health
Plant-based diets are often rich in:
- Antioxidants
- Fiber
- Polyphenols
- Healthy plant fats
- Magnesium and potassium
These nutrients have been linked to numerous cardiovascular benefits, including:
- Reduced arterial stiffness
- Improved cholesterol levels
- Lower inflammation
- Better metabolic health
- Enhanced endothelial function
While the term “plant-based” is sometimes misunderstood or overgeneralized, this study reinforces the importance of whole plant foods rather than processed substitutes. Ultra-processed plant-based products may not offer the same heart-protective qualities.
A Step Toward Human Trials
Because this study was performed in rats, the authors acknowledge the need for clinical trials in humans. However, since the diets used were made of foods commonly eaten by people, the pathway to testing these effects in clinical settings is straightforward. The researchers aim to conduct such trials next.
Research Paper Link
Prevention and Reversal of Hypertension-Induced Coronary Microvascular Dysfunction by a Plant-Based Diet (Journal of the American Heart Association, 2025)
https://doi.org/10.1161/jaha.125.045515