Blocking the FAM20C Gene Shows Big Metabolic Benefits in Obese Mice Without Any Weight Loss

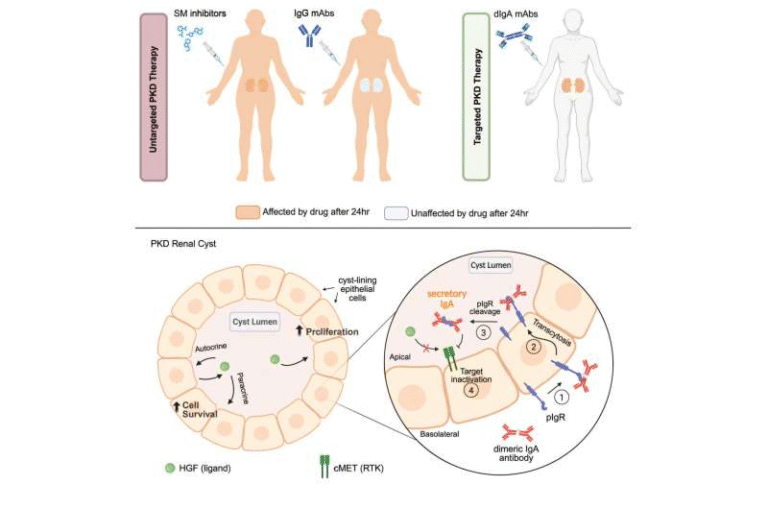
Researchers at Weill Cornell Medicine have uncovered a major early trigger behind inflammation in fat tissue, offering fresh insight into why some people with obesity develop type 2 diabetes, while others remain metabolically healthy. Their discovery centers on a protein called FAM20C, which appears to act like a biological switch that turns normal fat cells into inflammation-producing, insulin-resistant cells. And here’s the remarkable part: blocking this single gene in obese mice made them significantly healthier without reducing their body weight.
This straightforward study—published in the Journal of Clinical Investigation—adds an important new layer to our understanding of obesity-related diseases and could pave the way for a new class of treatments aimed at improving metabolic health even when weight loss is slow, difficult or incomplete.
What Exactly Is FAM20C and Why Does It Matter?
FAM20C is a kinase, a type of protein that modifies other proteins by adding phosphate groups. This chemical action can switch genes on or off, activate signaling pathways and lead to big downstream effects on cell behavior.
In the context of obesity, researchers noticed that FAM20C levels increase dramatically in fat cells, particularly in conditions where inflammation is already present. When this happens, fat cells begin releasing harmful inflammatory molecules. These same cells also become insulin resistant, which is one of the earliest steps toward developing type 2 diabetes.
The research team identified FAM20C by comparing gene activity in normal mice and mice with obesity and inflammation. FAM20C stood out because its activation pattern matched the development of fat-tissue inflammation. That made it a strong candidate for further testing—and the follow-up confirmed the suspicion.
What Happened When Scientists Increased FAM20C in Fat Cells?
When the researchers artificially increased FAM20C inside adipocytes (fat cells), two major effects appeared:
- The fat cells released large amounts of inflammatory molecules
- They became insulin resistant
This showed that boosting FAM20C is enough to trigger unhealthy metabolic changes on its own.
Even more importantly, these results confirmed that FAM20C isn’t a bystander—it is an active driver of metabolic dysfunction. That makes it a highly attractive therapeutic target.
Blocking FAM20C Transformed the Mice’s Health (But Not Their Weight)
This is where things get even more interesting.
Researchers genetically removed or blocked the FAM20C gene in the fat cells of obese mice. The mice did not lose any weight, but several major improvements occurred anyway:
- Sharper insulin sensitivity
- Reduced inflammation in fat tissue
- Better overall metabolic health
- Reduction of harmful visceral fat (the deep belly fat that surrounds organs)
Visceral fat is strongly associated with diabetes, fatty liver disease and heart disease. The fact that visceral fat decreased even without weight loss suggests that FAM20C is involved in how fat tissue “behaves,” not how much of it exists.
This distinction—fat quality vs. fat quantity—is becoming increasingly important in obesity science.
Does This Apply to Humans Too?
To find out, the team analyzed visceral fat samples from humans with obesity. The pattern was very similar:
- Individuals with high FAM20C levels showed greater insulin resistance
- People who were overweight or obese but had lower FAM20C levels tended to have better metabolic profiles
This provides early evidence that the fat-cell inflammation mechanism seen in mice is relevant to human metabolic disease as well.
It also sheds light on a long-standing mystery: why some individuals with obesity stay metabolically healthy for years, while others quickly develop diabetes and cardiovascular disease. Differences in FAM20C signaling could be part of that explanation.
A Deeper Look at the FAM20C Pathway
FAM20C doesn’t act alone. The protein modifies a variety of secreted molecules that influence other cells and tissues. Among these downstream targets is CNPY4, a protein identified as a key player in activating inflammatory gene programs inside adipocytes.
The research team highlighted CNPY4 as a major priority for future studies. Understanding how CNPY4 works could reveal additional intervention points to block inflammation before it spirals into insulin resistance.
FAM20C appears to interact with a wide network of proteins involved in:
- Metabolism
- Extracellular matrix remodeling
- Immune-system signaling
- Organ-to-organ communication
This fits with what scientists already know about FAM20C from broader biological research—it is considered a major kinase of the secretory pathway, meaning it influences proteins that are sent out of the cell and involved in diverse physiological processes.
Why This Discovery Is a Big Deal
One of the biggest challenges in treating metabolic disease is that weight loss, while beneficial, is often slow, incomplete or difficult to maintain. Many people remain insulin resistant or inflamed even after reducing body weight.
A treatment that improves metabolic health independently of weight loss would be a game-changer.
Blocking FAM20C—or interfering with its downstream effect on CNPY4—might eventually lead to:
- Better insulin sensitivity
- Lower inflammation
- Reduction of visceral fat
- Prevention or delay of type 2 diabetes
- Improved blood sugar control
- Protection against heart disease and fatty liver disease
The researchers specifically mentioned plans to develop small-molecule therapies targeting FAM20C or CNPY4. These drugs could be combined with weight-loss medications or used for people who do not respond fully to lifestyle changes.
A medication that improves metabolic health without requiring weight loss could help millions.
Broader Context: Why Fat-Cell Inflammation Is So Important
To understand why this research matters, it helps to step back and look at the bigger picture of adipose biology.
Fat Cells Aren’t Just Storage Units
Adipose tissue is a dynamic organ. Fat cells release hormones, immune molecules and signaling proteins that affect:
- Appetite
- Blood sugar control
- Liver function
- Muscle metabolism
- Immune responses
When fat cells become stressed or enlarged during obesity, they start releasing pro-inflammatory molecules. This inflammation disrupts insulin signaling and can spread throughout the body.
Not All Body Fat Is Equal
Visceral fat—the deep fat around organs—is more biologically active and more dangerous than subcutaneous fat near the skin. It releases more inflammatory mediators and is strongly associated with:
- Type 2 diabetes
- Heart disease
- Fatty liver disease
- High blood pressure
The fact that blocking FAM20C reduces visceral fat specifically is an important breakthrough.
Metabolically Healthy Obesity Exists
Some people with obesity have lower inflammation and better insulin sensitivity. They remain healthier for longer. Understanding why this happens could lead to targeted therapies that mimic that protective effect.
FAM20C may be one of the molecular switches that explains these differences.
What Comes Next?
The research team plans to:
- Examine how FAM20C affects other organs involved in metabolism, such as the liver and cardiovascular system
- Study CNPY4 in detail to determine its exact role in insulin resistance
- Begin exploring drug candidates that block FAM20C or its downstream targets
If these efforts succeed, future treatments could help people manage metabolic disease even when weight loss is limited.
Research Reference:
Secretory kinase FAM20C triggers adipocyte dysfunction inciting insulin resistance and inflammation in obesity
https://www.jci.org/articles/view/191075