Psychedelic Decriminalization Has Not Led to More Emergency Room Visits, According to a Major 2016–2023 Study

A new national analysis covering 2016 to 2023 offers one of the clearest looks yet at how changing psychedelic policies relate to public health. The findings are surprisingly steady: despite rising interest in substances like psilocybin and growing decriminalization efforts across the United States, hospital and emergency room admissions linked to hallucinogens have not increased. In fact, they declined after early 2020 and then stabilized, even as more municipalities and states reduced penalties for using or possessing psychedelics.
The study, published in JAMA Network Open, examined nationwide hospital-admission data using large insurance databases (including commercial and Medicaid records) to determine whether psychedelic decriminalization has contributed to more people seeking emergency or inpatient care. Based on all available evidence from 2016 through 2023, the answer appears to be no.
What the Researchers Actually Found
Across roughly 1.35 million substance-related hospital admissions recorded in the dataset, only about 21,700 cases—around 1.6%—involved hallucinogens. Month-to-month, hallucinogen-related admissions represented just 0.6% to 1.2% of all substance-linked encounters. That means that despite headline-grabbing attention around psychedelics, these drugs remain a relatively tiny contributor to emergency medical systems when compared to substances like alcohol and opioids, which dwarf hallucinogens in terms of harm and hospitalizations.
The data shows two distinct phases:
- 2016 to early 2020: A slow rise in hallucinogen-related admissions.
- Early 2020 to 2023: A steady decline, followed by stabilization.
This decline occurred even as more cities and states introduced decriminalization measures. The research team—including contributors from Saint Louis University, Washington University School of Medicine, and biostatisticians working with AHEAD—found no statistical connection between these policy changes and increases in hospital or ER visits.
Who Ends Up in the Hospital—and Why It Matters
The study also examined the characteristics of patients who required hospital care for hallucinogen-related issues. Among individuals with at least six months of continuous insurance enrollment before their admission:
- 35% had mood disorders
- 29.2% had anxiety disorders
- 14.7% had schizophrenia-spectrum disorders
- 18.9% had other substance-use disorders, such as alcohol, opioids, stimulants, cannabis, or sedatives
These numbers suggest that most hospitalizations linked to hallucinogens occur not among the general public experimenting with psychedelics, but among individuals already managing mental-health challenges or polysubstance use. This aligns with long-standing clinical knowledge that psychedelics can trigger or worsen psychological instability in vulnerable populations.
Importantly, the researchers emphasized that no evidence suggests widespread harm or increased ER burden following decriminalization. However, this doesn’t mean psychedelics are harmless—particularly for people with serious mental illness or those combining substances. The risks still exist, but the scale of those incidents remains small compared to other drugs.
Why This Study Stands Out
Several aspects make this research unusually valuable:
- National scope:
The study uses broad U.S. data rather than focusing on a single state or municipality. This helps clarify trends that might be obscured by local variation. - Seven years of data:
Covering 2016–2023 provides a long-term picture that captures both the pre-decriminalization era and the period during which psychedelic policy began shifting. - Comparison with other substances:
While psychedelic-related admissions stayed low and even declined, alcohol and opioids continued to dominate hospital visits. This sharp contrast helps highlight where the true public health burdens lie. - Policy relevance:
As psilocybin approaches potential FDA approval for treatment-resistant depression, understanding real-world safety trends becomes critical. This study adds evidence that increased psychedelic visibility has not triggered a spike in medical emergencies.
Important Limitations You Should Know
Even though the results are encouraging, there are several limitations worth acknowledging:
- All hallucinogens are grouped together.
The ICD-10 F16 diagnostic category includes classical psychedelics like psilocybin and LSD, but also other hallucinogenic substances such as ketamine. This makes it impossible to know which specific drugs contributed to the recorded admissions. - No geographic tracking.
Because the dataset lacks location identifiers, the research can’t link changes in admissions to specific decriminalized areas. Local effects—whether positive or negative—could be hidden within national averages. - Potential underreporting.
Hallucinogen-related diagnoses may be miscoded or missed entirely, simply because clinicians are more accustomed to documenting issues related to alcohol or opioids. - Hospital visits represent only one type of harm.
The study does not account for non-hospital adverse effects such as panic reactions, psychological distress, or longer-term consequences that do not require ER treatment.
Despite these limitations, the authors conclude that there is no sign of a broad public health problem emerging from psychedelic policy changes.
Additional Context: Why Psychedelic Use Has Been Increasing
Interest in psychedelics has surged over the past decade due to several developments:
- Growing scientific evidence supporting psilocybin’s potential benefits for depression, anxiety, addiction, and end-of-life distress.
- Media coverage painting psychedelics as a promising “new frontier” in mental health.
- Policy reform movements, especially in cities like Denver, Oakland, and Seattle, and statewide efforts in Oregon and Colorado.
- Cultural shifts, with younger adults showing more openness toward substances once viewed solely as recreational or dangerous.
As use becomes more common, the question of whether these substances contribute to increased emergency room visits becomes more important. So far, based on this extensive 2016–2023 dataset, the answer appears reassuring.
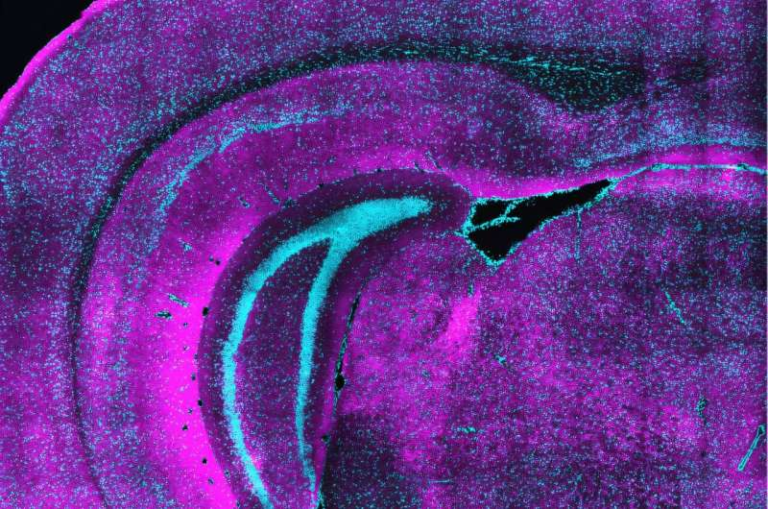
Broader Background: How Psychedelics Affect the Brain
Since part of this article is also meant to help readers learn something new, here’s a quick factual overview explaining why psychedelics can cause both profound experiences and, in rare cases, hospitalizations.
Classic psychedelics such as LSD, psilocybin, and DMT primarily act on serotonin 5-HT2A receptors in the brain. This interaction can temporarily alter:
- perception
- sensory processing
- mood
- sense of self
- time and spatial awareness
When used in supportive environments by mentally stable individuals, these effects are often reported as meaningful or transformative. But in unsafe contexts—or among individuals with conditions like schizophrenia—they can trigger confusion, panic, paranoia, or dangerous behavior, which occasionally leads to ER visits.
Unlike opioids or alcohol, psychedelics do not cause fatal overdose in normal circumstances, and they are not chemically addictive. This helps explain why their hospital-admission numbers are far lower than those of other substances.
Looking Ahead: What This Study Means for Policy and Public Health
As the United States continues to experiment with local decriminalization and potential therapeutic legalization, having strong empirical evidence is crucial. This seven-year analysis suggests:
- Psychedelic decriminalization has not created a meaningful rise in hospital demand.
- Heavy public health burdens continue to come from alcohol and opioids, not psychedelics.
- Future monitoring is still needed, especially in communities with changing laws.
- Individuals with mental-health disorders or other substance-use issues remain the most vulnerable to adverse reactions.
Overall, the study provides a grounded, data-driven counterpoint to fears that psychedelic reforms would overwhelm hospitals—something that has simply not happened on a national scale.
Research Paper:
Trends in Hallucinogen-Related Emergency Department and Hospital Admissions, 2016 to 2023
https://doi.org/10.1001/jamanetworkopen.2025.43453