Bone-Targeted Estrogen Delivery Shows Promise for Reversing Postmenopausal Osteoporosis Without Uterine Side Effects

Researchers have developed a new bone-targeted estrogen delivery system that could significantly improve treatment for postmenopausal osteoporosis—a condition that weakens bones and makes them prone to fractures. What makes this approach especially interesting is that it aims to provide the bone-protective benefits of estrogen while avoiding one of the biggest drawbacks of traditional hormone therapies: the risk of uterine and endometrial side effects.
This new method, tested in mice, uses a specialized two-layer coating that allows the hormone estradiol to travel through the body without interacting with organs like the uterus. Instead, it only becomes active once it reaches areas of weakened bone. Early findings show that this strategy not only restored bone density but actually raised it above pre-osteoporosis levels, all without causing harmful effects to reproductive tissues.
Understanding Why Estrogen Matters for Bone Health
After menopause, the body’s estrogen levels decline sharply. Estrogen plays a key role in maintaining bone health by reducing bone resorption (the breakdown of bone tissue) and supporting bone formation. When estrogen levels fall, bones become more fragile, leading to postmenopausal osteoporosis.
Traditional treatment often involves giving estradiol to replace what the body no longer produces. But a major problem is that most estradiol is metabolized before reaching the bones—and whatever remains can stimulate the lining of the uterus, potentially increasing the risk of endometrial hyperplasia and cancer. This risk has limited widespread long-term use of estrogen for bone protection.
This is where the new research becomes especially relevant.
How the New Delivery System Works
Scientists Xi Chen, Changsheng Liu, and Jiajing Zhou designed a system that encapsulates estradiol inside a structure engineered to recognize and respond to the environment of osteoporotic bone.
The system uses two key components:
- Peptide Coating
The estradiol is first coated with peptides that have a natural attraction to calcium ions, which are abundant in bone. This helps pull the hormone directly to skeletal tissue. - Metal–Phenolic Network (MPN) Outer Shell
The peptide-coated hormone is then placed inside a tiny cage-like shell made of:- Tannic acid (TA) – A compound that helps block bone-resorbing cells.
- Magnesium ions (Mg²⁺) – Important for improving bone structure and encouraging the growth of bone-building cells.
This outer shell remains stable in neutral pH (like in the bloodstream), but it dissolves in acidic environments, which are typical of bones undergoing resorption or degradation. This means the estradiol is only released where bones are weakened—providing a targeted effect.
The release mechanism also delivers TA and Mg²⁺ directly into damaged bone areas, giving the therapy multiple benefits at once.
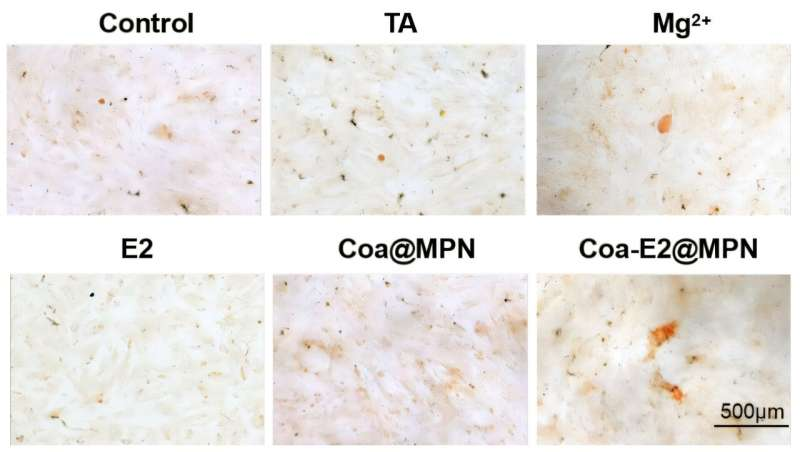
What Lab Tests Found
Before moving to animal studies, researchers examined how the encapsulated estradiol behaved in lab conditions:
- In neutral solutions, the caged molecules stayed intact.
- In acidic solutions, similar to the microenvironment of osteoporotic bone, the shell dissolved and released:
- Estradiol
- Magnesium ions
- Tannic acid
These results showed that the system was both stable and responsive—exactly what targeted therapy requires.
What the Animal Study Showed
The research team tested the delivery system in mice with postmenopausal osteoporosis. The mice were separated into groups and given:
- The new caged estradiol
- Regular estradiol
- A saline solution
Treatments were administered twice a week for four weeks.
The mice that received the bone-targeted estradiol showed dramatic improvement:
- Bone density rose above pre-osteoporosis levels
- No uterine enlargement or other reproductive side effects were detected
- Fluorescence imaging confirmed that the estradiol localized solely in weakened bones
The untreated and regular estradiol groups did not display the same favorable combination of bone improvement and lack of side effects.
This makes the new method particularly compelling: it retains the strength of estrogen therapy while removing its biggest long-term safety concern.
Why This Could Be a Major Development
This drug-delivery strategy may represent a new direction for hormone-based treatments. Instead of flooding the whole body with estrogen—which increases risks to reproductive organs and sometimes other tissues—this system delivers just enough hormone, exactly where it is needed, and only when the surrounding conditions trigger release.
The researchers emphasize that this design is not only effective but also safer. Because it prevents estrogen from interacting with the uterus, it could become a viable long-term solution for women who cannot take standard estrogen therapy.
They also mentioned future plans to develop an oral version of this double-coated estradiol system, which would be significantly easier for patients to use.
Additional Background: Why Targeted Therapies Are Becoming Important
Postmenopausal osteoporosis affects millions worldwide. While treatments such as bisphosphonates, selective estrogen receptor modulators (SERMs), and parathyroid hormone analogs exist, each has limitations:
- Bisphosphonates may cause gastrointestinal issues or rare complications like jaw necrosis.
- SERMs do not offer the same bone-building effects as estrogen.
- Parathyroid hormone treatments can be expensive and inconvenient.
Meanwhile, estrogen remains one of the most effective and natural treatments for bone loss—but systemic risks overshadow its benefits.
A targeted estrogen therapy therefore fits into a larger trend in medicine: precision delivery, where drugs impact only the tissues that need them.
The new MPN-coated coacervate system also aligns with a growing understanding that bones are dynamic, cellular structures influenced by hormones, pH changes, and biochemical signals. By responding to the acidic microenvironment of active bone resorption, this system uses the body’s own signals to trigger release—something traditional pills or injections cannot do.
The Role of Magnesium and Tannic Acid
This research goes beyond simply delivering estradiol. The additional materials in the coating—tannic acid and magnesium ions—contribute to the therapy in unique ways.
- Magnesium plays a crucial role in bone mineralization and supports osteoblast activity. Deficiency in magnesium has long been associated with weaker bone structure.
- Tannic acid, a polyphenol, can naturally inhibit osteoclast activity, helping reduce the rate at which bone is broken down.
By incorporating these into the outer shell, the system does more than restore hormone levels—it also supports bone regeneration and reduces bone degradation.
How This Fits Into the Future of Osteoporosis Treatment
While these results are extremely promising, they are still early-stage. The therapy has only been tested in mice, and translating such technologies to human use often takes years of additional research, safety testing, and clinical trials.
But the concept itself—bone-targeted hormone delivery—opens the door to:
- Safer estrogen therapies
- Combination drug-release systems
- Microenvironment-responsive medicine
- Multifunctional coatings that support tissue repair
If eventually approved for human use, this could become a meaningful option for women entering menopause who want to protect their bone health without taking on the risks associated with systemic estrogen therapy.
Research Paper
A Metal–Phenolic Network-Coated Coacervate System Mediates Mitochondrial Modulation and Bone Homeostasis Restoration for Postmenopausal Osteoporosis Therapy
https://doi.org/10.1021/acs.nanolett.5c04029