In-Home Sensor Technology Is Bringing Smarter, Real-Time Care to People Living With ALS
Amyotrophic lateral sclerosis, commonly known as ALS, is one of the most challenging neurodegenerative diseases to manage. It gradually damages the nerve cells responsible for controlling voluntary muscles, leading to worsening difficulties with movement, speech, swallowing, and breathing. One of the biggest challenges for both patients and clinicians is that ALS does not progress the same way for everyone. Some people experience rapid decline, while others lose function more slowly, making it difficult to predict when care needs to change.
Researchers at the University of Missouri are now working on a solution that could significantly improve how ALS progression is tracked and managed. By combining in-home sensor technology with artificial intelligence, they are developing a system that continuously monitors daily health changes and provides clinicians with actionable insights—well before serious problems arise.
Why Monitoring ALS Between Clinic Visits Is a Major Problem
ALS care today relies heavily on periodic clinic visits, where clinicians assess patients using standardized tools. One of the most important of these tools is the ALS Functional Rating Scale Revised (ALSFRS-R). This scale measures how well a person can perform everyday activities such as walking, speaking, eating, and breathing. While it is clinically valuable, it only captures a snapshot of the patient’s condition at the time of the visit.
Between appointments, clinicians often have very limited visibility into how a patient’s health is changing. Subtle declines in balance, sleep quality, or breathing patterns can go unnoticed until they lead to serious consequences like falls, respiratory complications, or hospitalizations. This gap in monitoring is what the University of Missouri team aims to close.
How In-Home Sensors Are Being Used
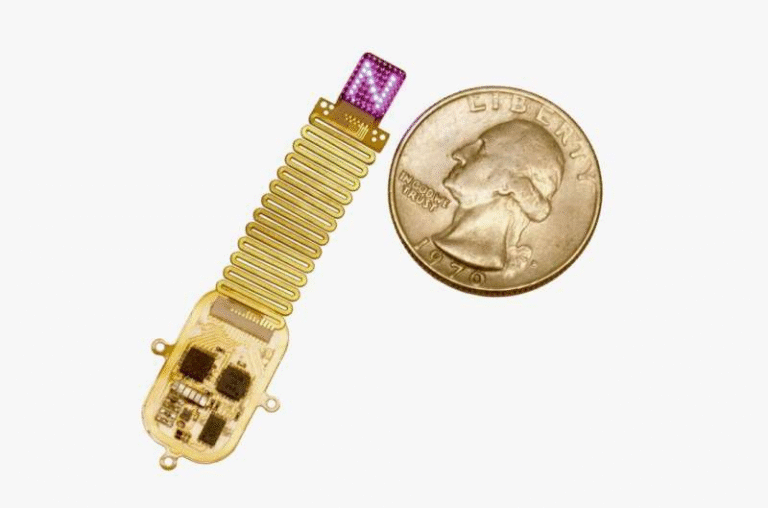
The project adapts ambient, contact-free sensors that were originally designed to monitor older adults living independently at home. These sensors do not require wearable devices or cameras. Instead, they quietly collect data about daily routines and physical behaviors.
The system can detect changes in:
- Walking and mobility patterns
- Overall movement levels
- Sleep duration and sleep quality
- Daily activity rhythms
- Behavioral changes that may signal functional decline
For people with ALS, whose physical abilities may decline faster and less predictably than in typical aging, this kind of continuous monitoring provides a much clearer picture of real-world function.
From Raw Sensor Data to Meaningful Health Insights
Collecting data is only part of the solution. The real innovation lies in how the data is analyzed. The sensor data is transmitted wirelessly through two small in-home devices and securely transferred to university systems. There, researchers apply machine learning models to interpret the information.
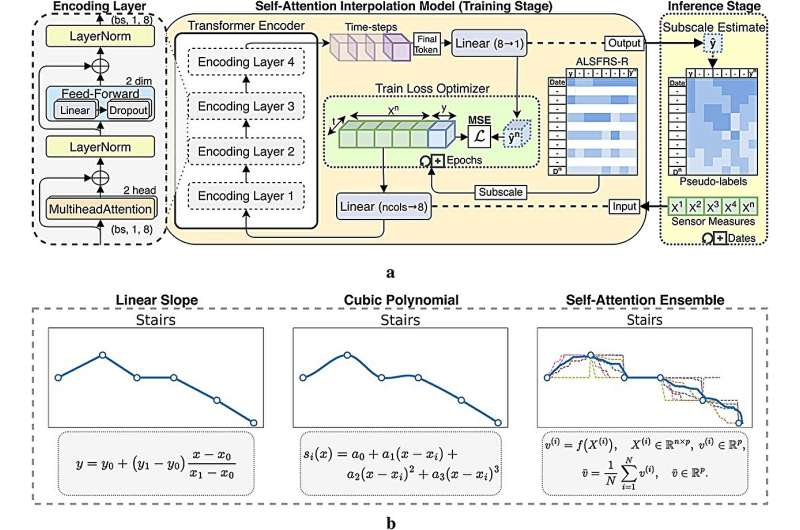
The models are designed to estimate a patient’s ALSFRS-R score based on sensor-derived patterns. Instead of relying solely on clinician-entered scores during visits, the system can generate semi-supervised estimates of functional ability over time. This approach allows researchers to track progression on a near-daily basis.
A key part of the study involves validating that sensor-based estimates truly reflect what patients experience in their daily lives. Once verified, the system can move beyond tracking and into predictive modeling, identifying trends that may signal future problems.
Predicting Problems Before They Become Crises
One of the most promising aspects of this technology is its ability to detect changes before patients themselves may notice them. For example, small alterations in gait could indicate increasing weakness or balance issues. Subtle changes in nighttime movement or respiration could suggest emerging breathing difficulties.
By identifying these patterns early, clinicians could:
- Intervene before a fall occurs
- Adjust medications sooner
- Recommend assistive devices at the right time
- Prevent avoidable hospital admissions
The goal is not just to react to decline, but to anticipate it.
Integrating Sensor Data Into Clinical Care
The research team plans to integrate this monitoring system directly into clinical workflows. In future implementations, clinicians could access a secure digital portal showing a patient’s daily health trends, similar to how intensive care units monitor vital signs in real time.
If the system predicts a concerning decline, it could automatically trigger an alert for the care team. This allows healthcare providers to reach out proactively, rather than waiting for the next scheduled visit or emergency event.
Early feedback from participating families suggests that this approach offers peace of mind, helping patients feel more connected to their care teams even while living at home.
Protecting Privacy While Using Smart Technology
Privacy is a critical concern when monitoring health in personal living spaces. The researchers emphasize that the system is designed with security and discretion in mind. The sensors do not capture images or audio, and all transmitted data is securely handled within university research systems.
By focusing on movement and behavior patterns rather than direct observation, the technology balances innovation with respect for personal privacy.
The Science Behind the Study
The research, titled “Enhancing ALS progression tracking with semi-supervised ALSFRS-R scores estimated from ambient home health monitoring,” explores how interpolation techniques and self-attention transformer models can be applied to incomplete clinical data. These techniques allow researchers to estimate ALSFRS-R subscores even when labeled clinical data is limited.
The study demonstrates how semi-supervised learning can bridge the gap between sparse clinic assessments and continuous real-world data, improving the accuracy and usefulness of progression tracking.
Beyond ALS: A Broader Impact on Chronic Disease Care
While this project focuses specifically on ALS, the implications extend much further. The same combination of ambient sensors and AI-driven analysis could be adapted for other chronic and progressive conditions, including:
- Parkinson’s disease
- Heart failure
- Other neurological or mobility-limiting disorders
As healthcare increasingly shifts toward remote patient monitoring, technologies like this could play a major role in keeping people healthier at home while reducing strain on healthcare systems.
A Smarter Way Forward for ALS Care
ALS remains an incurable disease, but better monitoring can significantly improve how it is managed. By providing continuous, real-time insights into daily function, in-home sensor technology offers a smarter, more responsive approach to care. It empowers clinicians with better data, supports patients and families with timely interventions, and represents a meaningful step toward more personalized, proactive healthcare.
As this research continues to evolve, it may redefine how ALS progression—and chronic disease care more broadly—is monitored in the years ahead.
Research paper:
https://www.frontiersin.org/articles/10.3389/fdgth.2025.1657749/full