A New Algorithm Could Make Stroke Detection Scans Faster, Portable, and Far More Accessible
Researchers at NYU Tandon School of Engineering have unveiled a powerful new algorithm that could dramatically change how strokes are diagnosed, especially in places where traditional imaging tools are unavailable. The breakthrough focuses on microwave-based brain imaging, a technology long seen as promising but held back by one major problem: speed. With this new approach, image reconstruction times that once took close to an hour can now be reduced to under 40 seconds, bringing real-time stroke detection much closer to reality.
Why Speed Matters in Stroke Diagnosis
When a patient arrives with symptoms of a stroke, doctors must quickly determine whether the stroke is caused by a blood clot (ischemic stroke) or bleeding in the brain (hemorrhagic stroke). The treatments for these two conditions are completely different, and giving the wrong one can be fatal. Today, this distinction is usually made using CT scans, which are large, expensive, stationary machines that require shielded rooms and trained operators.
This dependence on CT scanners creates a serious gap in care. Ambulances, rural clinics, and many hospitals worldwide simply do not have access to this equipment. As a result, patients may lose precious time while being transported to facilities that can perform these scans. Every minute matters, and delays can mean the difference between recovery, long-term disability, or death.
The Promise of Microwave Brain Imaging
For years, scientists have explored the idea of using microwave imaging as an alternative. This technology works by sending low-power microwave signals into the head and measuring how they scatter. Because different tissues—healthy brain tissue, blood, swelling, or tumors—have different electrical properties, microwaves can detect these differences without using radiation.
The vision has been compelling: a lightweight, portable imaging device, possibly no larger than a bike helmet, that could be used in ambulances or small clinics. Such a device would not require radiation shielding or massive infrastructure, making it safer and far more accessible.
The hardware for this idea already exists. The true bottleneck has always been the computational process required to turn raw microwave data into a usable image of the brain.
The Computational Roadblock
Traditional microwave imaging relies on complex mathematical models that repeatedly estimate the electrical properties of tissues, simulate how microwaves would behave under those conditions, and then adjust the estimates again. This process can involve solving large electromagnetic equations hundreds of times, making it painfully slow.
Even with modern computing power, reconstructions could take up to an hour. That timeline makes the technology impractical for emergency medicine, where clinicians cannot afford to wait.
A Smarter Way to Reconstruct Images
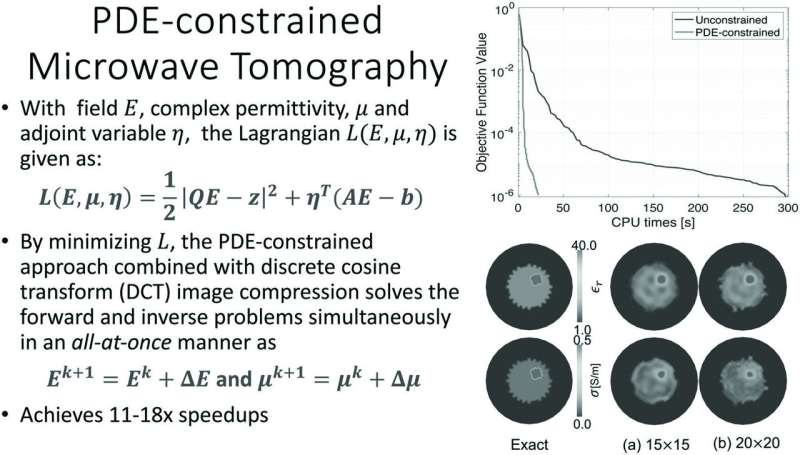
The NYU Tandon research team, led by Stephen H. Kim, alongside Lara Pinar and Andreas Hielscher, approached the problem from a different angle. Instead of trying to make each intermediate step perfectly accurate, their new algorithm allows quick, imperfect approximations early on, refining accuracy only when it becomes truly necessary.
This change in strategy dramatically reduces the number of heavy computations required. The team also introduced several additional optimizations, including:
- A compact mathematical representation that shrinks the overall problem size
- More efficient methods for updating calculations between iterations
- A modeling approach that remains stable even for complex head shapes, which is crucial for real-world medical use
Together, these improvements allow the algorithm to converge on high-quality images far faster than previous methods.
Real-World Testing and Results
The results are striking. Reconstructions that once took nearly an hour can now be completed in seconds rather than minutes, often in less than 40 seconds. The algorithm achieved speed improvements of 10 to 30 times compared to the best existing techniques.
Importantly, this wasn’t just a theoretical or simulated success. The researchers tested their method using real experimental data, including cylindrical targets scanned with a microwave imaging system developed at the University of Manitoba. In these tests, the algorithm consistently delivered high-quality reconstructions with dramatically reduced processing times.
Why This Is a Turning Point
This breakthrough does not depend on new hardware or faster computers. Instead, it comes from rethinking the mathematics behind microwave image reconstruction. For researchers who have worked in this field for decades, this represents a long-awaited shift.
By solving the speed problem, microwave imaging can finally move beyond laboratory demonstrations and toward real clinical environments. Portable, affordable imaging systems become far more realistic when image reconstruction happens fast enough to support urgent medical decisions.
Beyond Stroke Detection
While stroke diagnosis is one of the most urgent and obvious applications, the implications of this work go much further. Portable microwave imaging could eventually be used to:
- Monitor brain swelling in intensive care units without repeated CT scans
- Provide a low-cost alternative to mammography in regions with limited access to breast cancer screening
- Track tumor response to therapy by detecting subtle changes in tissue composition over time
Because microwave imaging does not rely on ionizing radiation, it could also be safer for repeated use, making it especially valuable for long-term monitoring.
What Comes Next
The research team is now focused on extending their algorithm to full 3D imaging, a necessary step for widespread clinical adoption. Three-dimensional reconstructions would provide clinicians with more detailed and clinically relevant information, further closing the gap between experimental systems and practical medical tools.
With faster algorithms now in place, the remaining challenges are largely about integration, validation, and deployment. If these hurdles are cleared, microwave imaging could soon play a meaningful role in emergency medicine, critical care, and global health.
A Step Toward More Equitable Stroke Care
One of the most important aspects of this breakthrough is its potential impact on healthcare access. Stroke is a global problem, and many regions lack the infrastructure required for advanced imaging. A portable, fast, and affordable imaging solution could help bring life-saving diagnostics to patients who currently have few options.
By dramatically reducing computation time, this new algorithm gives microwave imaging the speed it needs to matter clinically. It takes a technology that has been stuck on the sidelines and moves it closer to the front lines of patient care.
Research Reference:
Accelerated Microwave Tomographic Imaging With a PDE-Constrained Optimization Method – IEEE Transactions on Computational Imaging (2025)
https://doi.org/10.1109/TCI.2025.3629414