Why Nearly 40 Percent of GLP-1 Weight Loss Drug Prescriptions Are Never Filled Despite Insurance Coverage

Popular GLP-1 receptor agonist medications, widely known for their effectiveness in treating obesity and diabetes, are often described as game-changers. These drugs can help patients lose 10 to 20 percent of their body weight, improve blood sugar control, and reduce long-term health risks. Yet a new study reveals a surprising and concerning reality: about 40 percent of GLP-1 prescriptions are never filled, even when patients have health insurance.
This finding comes from a detailed analysis published in JAMA Health Forum and highlights how cost, insurance design, and systemic disparities continue to shape who actually benefits from these high-profile medications.
JAMA Health Forum, 2025
What the Study Looked At and Why It Matters
The research was led by Anna Sinaiko, an associate professor of health economics and policy at the Harvard T.H. Chan School of Public Health, along with collaborators from Harvard, the Harvard Pilgrim Health Care Institute, Brigham and Women’s Hospital, Duke University, and the University of Colorado.
The goal was simple but important: move beyond headlines about sticker prices and examine what really happens after a doctor writes a prescription. While public discussion has focused heavily on the full retail cost of GLP-1 drugs—often around $900 per month without insurance—much less was known about patient behavior when insurance is involved.
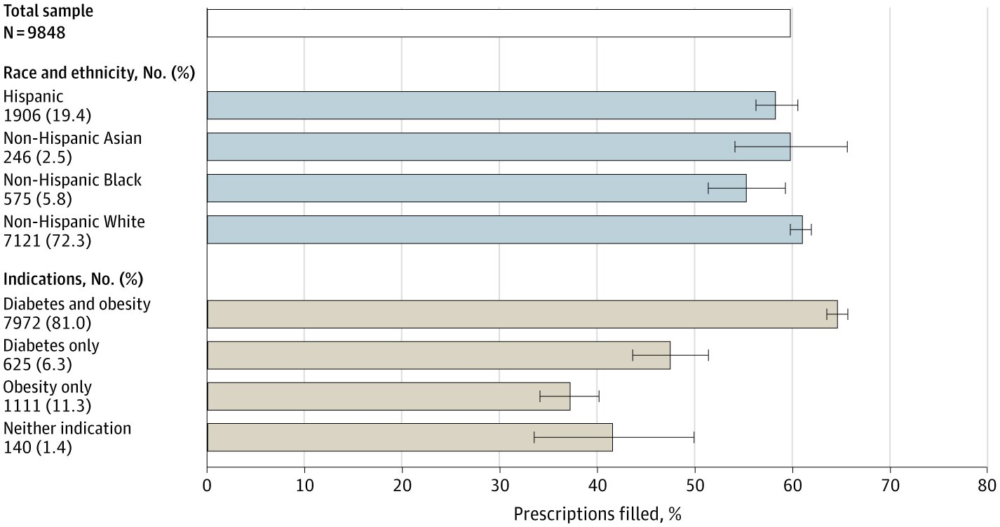
To answer that question, the researchers analyzed 9,848 GLP-1 prescription orders written for 6,094 patients. They linked electronic medical records from the University of Colorado Health System with pharmacy claims data, allowing them to track whether prescriptions were actually picked up.
The Headline Finding: A 60 Percent Fill Rate
The most striking result was that only 60.1 percent of GLP-1 prescriptions were filled. In other words, nearly four out of every ten prescriptions went unclaimed at the pharmacy.
This gap between prescribing and actual use is especially concerning given how effective these drugs can be. It also raises questions about whether simply prescribing a medication is enough to improve outcomes for chronic conditions like obesity and diabetes.
Clear Differences by Race and Ethnicity
The study also uncovered meaningful disparities in prescription fill rates across racial and ethnic groups:
- White patients filled 60.9 percent of their prescriptions
- Hispanic patients filled 58.4 percent
- Black patients filled only 55.3 percent
While the differences may appear modest at first glance, they reflect persistent inequities in access to care and affordability, even among insured patients. These patterns suggest that structural barriers don’t disappear once someone has coverage.
Out-of-Pocket Costs Still Add Up
One of the most revealing parts of the study involved out-of-pocket costs, which many people assume are minimal with insurance.
On average, patients who did fill their prescriptions paid $71.90 per month out of pocket. But this figure masked significant variation:
- Black patients paid an average of $41.15
- Hispanic patients paid $63.69
- White patients paid $78.37
Even though Black patients paid less on average, they were still less likely to fill their prescriptions, pointing to broader financial pressures and access issues beyond just the dollar amount.
Importantly, many prescriptions came with monthly costs close to $100, which can be a major burden for patients managing multiple medications or living on tight budgets.
Medical Condition Strongly Influenced Fill Rates
The likelihood of filling a GLP-1 prescription also depended heavily on why the drug was prescribed:
- Patients with both diabetes and obesity were the most likely to fill their prescriptions
- Those with diabetes only filled prescriptions at lower rates
- Patients with obesity only were the least likely to pick up their medication
This last group also faced the highest out-of-pocket costs, reinforcing the idea that insurance coverage for obesity treatment remains weaker and less consistent than coverage for diabetes.
Taken together, these patterns suggest that cost sensitivity and perceived medical necessity play a major role in whether patients follow through.
Why Are Prescriptions Going Unfilled?
The study could not directly measure patients’ reasons for leaving prescriptions unfilled. Factors such as concerns about side effects, uncertainty about long-term use, or hesitation around injectable medications may all play a role.
Still, the data strongly point toward affordability as a key driver. When patients with the greatest medical need and lowest costs are most likely to fill prescriptions, it becomes difficult to ignore the financial signal.
Even with insurance, paying $60 to $100 every month indefinitely can be unrealistic for many households.
What This Means for the Health Care System
The findings highlight two major challenges.
First, health disparities persist even within insured populations. Having coverage does not guarantee equal access to high-value medications, especially for racial and ethnic minority groups and lower-income patients.
Second, the study underscores the ongoing problem of medication nonadherence in chronic disease care. Obesity and diabetes require long-term management, and treatment only works if patients can realistically sustain it.
The researchers suggest that future studies should examine how clinicians respond when patients don’t pick up prescriptions—whether by switching to lower-cost options or adjusting treatment plans.
A Changing Market With Uncertain Impact
The GLP-1 drug market is evolving rapidly. New medications are being developed, and insurers are actively reconsidering coverage policies as costs rise. Many private insurers are expected to tighten access, limiting coverage to patients with diabetes or severe obesity.
In early November, President Donald Trump announced a pricing agreement with Eli Lilly and Novo Nordisk, makers of Zepbound and Wegovy, respectively. Under the deal, prices could drop to as low as $149 per month for Medicare, Medicaid, and self-paying patients.
While this represents a substantial reduction from retail prices, the study raises an important question: will it be enough? After all, many patients in the study chose not to fill prescriptions even when their costs were already lower than $149.
Why Affordability Remains the Central Issue
The takeaway from this research is clear. Affordability operates at multiple levels, and lowering headline prices alone may not solve access problems.
When nearly 40 percent of insured patients decide a medication is still too expensive—or too risky financially—to try, it suggests deeper structural issues in how prescription drugs are priced, covered, and delivered.
For high-impact medications like GLP-1s, improving access will likely require better insurance coverage, lower cost-sharing, and targeted policies aimed at reducing disparities, not just price announcements.