Estrogen May Be the Missing Link Explaining Why Women Experience More Gut Pain and IBS

Women are far more likely than men to suffer from irritable bowel syndrome (IBS), a chronic digestive disorder marked by abdominal pain, bloating, cramping, and altered bowel habits. For years, doctors and researchers have observed this gender gap, but the biological reason behind it has remained unclear. New research from scientists at the University of California, San Francisco (UCSF) now offers a detailed explanation, pointing to the hormone estrogen as a key driver of heightened gut pain sensitivity.
The study, published in the journal Science, reveals that estrogen activates previously unknown cellular pathways in the colon that amplify pain signaling. These findings not only help explain why IBS disproportionately affects women but also open the door to new treatment strategies that go beyond diet changes and symptom management.
How Estrogen Changes the Way the Gut Feels Pain
The gut has its own complex sensory system designed to detect chemical and mechanical changes and relay that information to the nervous system. The UCSF researchers discovered that estrogen can dial up this pain-sensing system, making the gut more reactive to everyday stimuli, including certain foods and their breakdown products.
In experiments with mice, researchers found that when male mice were given estrogen at levels comparable to those naturally present in females, their sensitivity to gut pain increased significantly. In fact, their pain responses became similar to those observed in female mice. This result strongly suggests that estrogen itself plays a direct and causal role in gut pain sensitivity rather than acting indirectly.
A Surprising Discovery Inside the Colon
To understand how estrogen was influencing gut pain, the research team first needed to identify where estrogen receptors are located in the intestine. Scientists had long assumed that estrogen mainly acted on enterochromaffin (EC) cells, which are known to release serotonin and send pain-related signals from the gut to the spinal cord.
Instead, the researchers were surprised to find that estrogen receptors were concentrated in the lower colon and primarily located on a different type of cell known as L-cells.
This unexpected discovery changed the entire understanding of how hormonal signaling affects gut pain.
The Newly Identified Pain Pathway
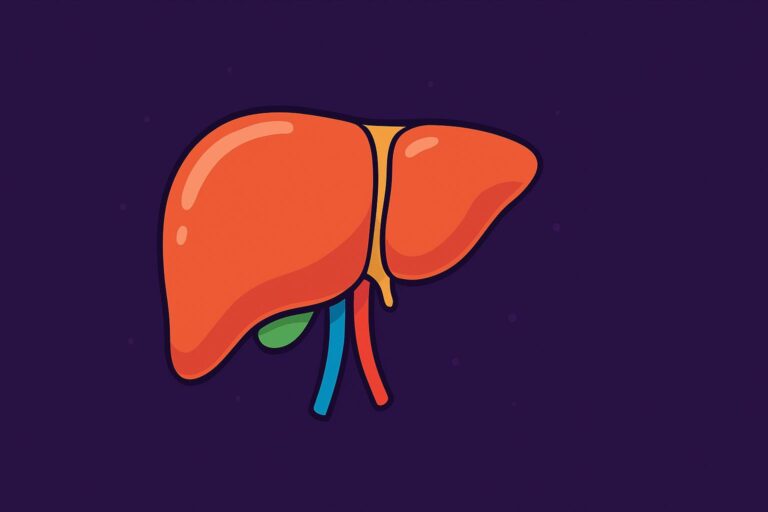
Once estrogen binds to receptors on L-cells, it sets off a multi-step chain reaction that ultimately increases pain signaling:
First, estrogen stimulates L-cells to release a hormone called PYY (peptide YY). PYY has traditionally been associated with appetite control and satiety, and for decades it was studied mainly for its role in suppressing hunger.
Next, PYY acts on nearby EC cells, prompting them to release serotonin, a neurotransmitter that plays a major role in gut motility and pain signaling.
Finally, serotonin activates pain-sensing nerve fibers that transmit signals from the gut to the nervous system, leading to heightened discomfort and pain.
In female mice, blocking any part of this pathway—by removing the ovaries, inhibiting estrogen signaling, or interfering with PYY or serotonin—dramatically reduced gut pain sensitivity. This provided strong evidence that the pathway is responsible for the higher baseline gut pain observed in females.
Why PYY’s Role Matters More Than We Thought
One of the most striking aspects of this research is the newly identified role of PYY as a pain signal. For years, pharmaceutical companies attempted to develop PYY-based drugs for weight loss, since the hormone reduces appetite. However, those trials consistently failed because participants experienced severe gastrointestinal discomfort.
At the time, the cause of that distress was unclear. The new findings offer a compelling explanation: elevated PYY levels may directly increase gut pain sensitivity, especially in the colon. This insight reframes how scientists think about PYY and highlights why earlier drug trials produced such problematic side effects.
The Diet Connection and the Role of Gut Bacteria
Estrogen does more than just increase PYY levels. The study also found that estrogen boosts the expression of a receptor called Olfr78 on L-cells.
Olfr78 detects short-chain fatty acids, which are molecules produced when gut bacteria ferment certain carbohydrates in the diet. These fatty acids are common byproducts of foods classified as FODMAPs—fermentable carbohydrates found in items like onions, garlic, wheat, beans, and some fruits.
With more Olfr78 receptors present, L-cells become hypersensitive to these bacterial metabolites. This makes the cells easier to activate, leading to even more PYY release and further amplification of pain signaling.
This “double hit” effect—higher baseline sensitivity from estrogen plus increased responsiveness to microbial metabolites—may explain why low-FODMAP diets help some people with IBS. By reducing the intake of fermentable carbohydrates, patients may be limiting the production of short-chain fatty acids that trigger this pain pathway.
Why IBS Symptoms Fluctuate Over Time
The findings also help explain several long-standing clinical observations. Many women with IBS report that their symptoms worsen during certain phases of the menstrual cycle, when estrogen levels fluctuate. Pregnancy, lactation, and hormonal contraceptive use may also influence gut sensitivity in similar ways.
Although men possess the same cellular pathway, their lower estrogen levels keep it relatively inactive. However, the pathway may become more active in men undergoing treatments that alter hormone balance, such as androgen-blocking therapies, which can raise estrogen levels and sometimes lead to digestive side effects.
What This Means for Future IBS Treatments
Current IBS treatments focus largely on managing symptoms through diet changes, stress reduction, and medications that target gut motility. While helpful, these approaches do not address the underlying biological drivers of pain.
The newly identified estrogen–PYY–serotonin pathway offers several promising drug targets. Medications that selectively block estrogen signaling in the gut, inhibit PYY’s pain-related effects, or interfere with Olfr78 activation could provide more precise and durable relief for IBS patients.
This is particularly important because low-FODMAP diets, while effective for some, are notoriously difficult to maintain long-term and may negatively impact gut microbiome diversity.
Broader Implications for Gut Health Research
Beyond IBS, this research underscores the importance of considering sex differences in medical research, especially in conditions involving pain perception. Hormones like estrogen clearly influence how the body processes sensory information, and ignoring these differences may limit the effectiveness of treatments.
The study also highlights the intricate relationship between hormones, gut cells, the microbiome, and the nervous system, reinforcing the idea that digestive health cannot be separated from broader physiological systems.
Research Reference
A cellular basis for heightened gut sensitivity in females
Published in Science (2025)
https://www.science.org/doi/10.1126/science.adz1398