Mental Health Conditions Are Strongly Linked to a Higher Risk of Unintentional Injuries, Major Study Finds
A growing body of research has long shown that mental health affects physical health, but a new large-scale study highlights a risk that has received far less attention: physical injuries, especially those that are unintentional. According to newly published findings from researchers at the University of Michigan, people living with mental health conditions face a significantly higher risk of injury than those without such conditions. These injuries range from falls and traffic accidents to self-harm and assault-related injuries.
The study, published in the journal Nature Mental Health, brings fresh attention to an overlooked public health issue and suggests that injury prevention should be a core part of mental health care, not a separate concern.
What the Study Looked At
To understand how mental health conditions influence injury risk, researchers analyzed population-wide administrative data from nearly five million individuals across Norway and New Zealand. This makes the study one of the largest and longest-running investigations of its kind.
Participants were followed for long periods, ranging from 14 to 30 years, allowing researchers to examine how mental health conditions affected injury risk over time rather than just at a single moment.
Mental health conditions were identified using:
- Primary care medical records
- Inpatient hospital records
Injuries were tracked using:
- Primary care records
- Hospital admissions
- Injury insurance claims
This broad data coverage allowed researchers to capture both minor and severe injuries, offering a comprehensive picture of injury risk.
Why Unintentional Injuries Matter
Injury is a major public health issue worldwide. Unintentional injuries—such as falls, vehicle crashes, and workplace accidents—account for the majority of injuries globally and are among the leading causes of premature death, especially in younger and middle-aged populations.
Despite this, most earlier research on mental health and injury has focused almost entirely on intentional injuries, such as suicide attempts or self-harm, and sometimes assault victimization. Very little attention had been paid to whether mental health conditions increase the risk of everyday accidental injuries.
The researchers behind this study aimed to fill that gap.
Key Findings From the Research
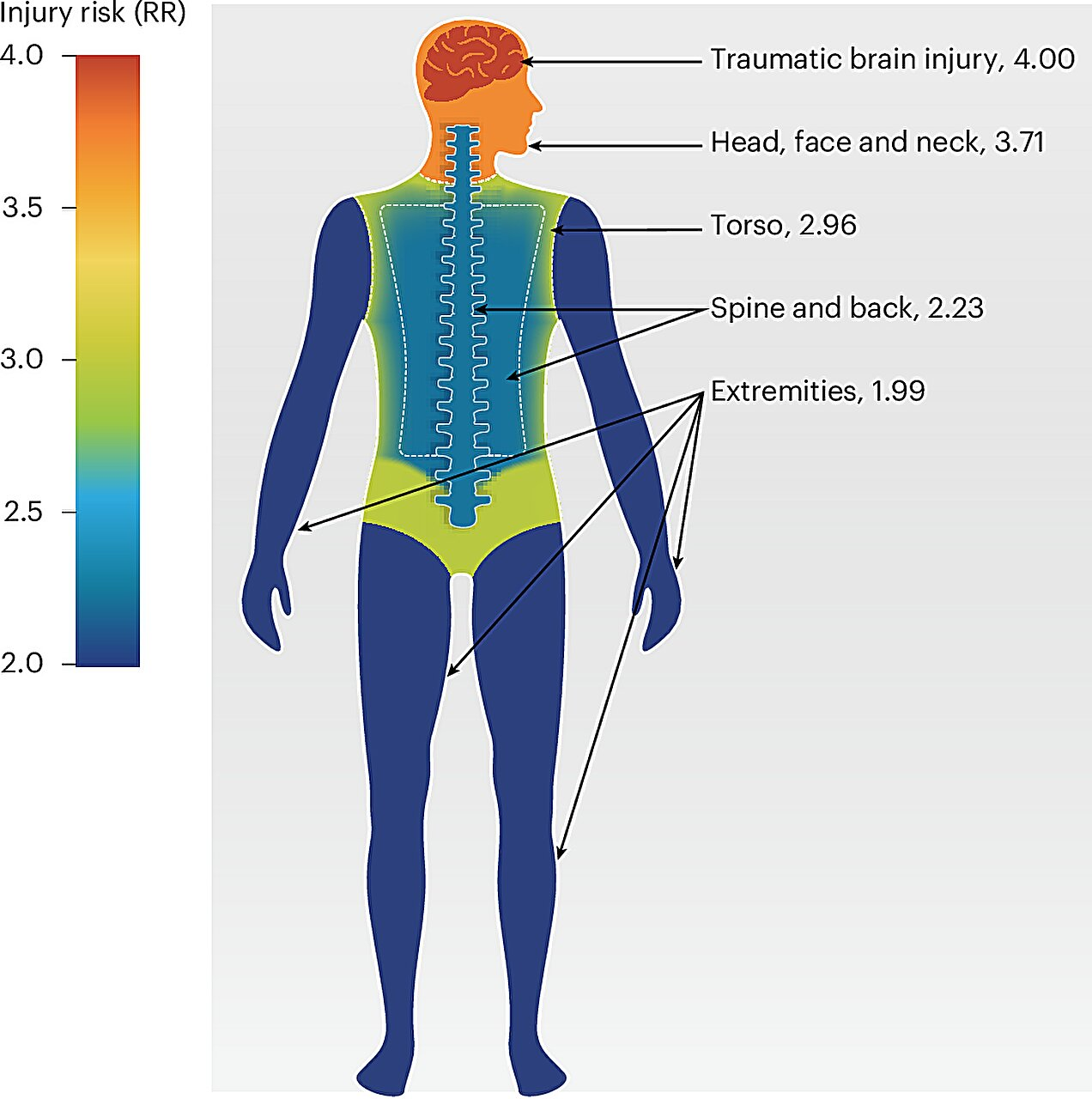
The results were clear and consistent. Individuals with mental health conditions showed elevated risks across multiple types of injury, including:
- Unintentional injuries, such as falls and traffic accidents
- Self-harm-related injuries
- Assault-related injuries
What stood out most was that the increased risk of unintentional injury was widespread, appearing across:
- Different mental health conditions
- Different types of injuries
- Different age groups and socioeconomic backgrounds
One particularly strong pattern emerged: injuries affecting the brain and head were especially common among individuals with mental health conditions.
Importantly, researchers ruled out several possible explanations. The higher injury risk could not be explained by preexisting injuries, nor could it be attributed solely to socioeconomic background. This suggests that mental health conditions themselves play a direct and meaningful role in increasing vulnerability to injury.
A Broader Range of Mental Health Conditions Are Involved
Another key takeaway is that this risk is not limited to severe psychiatric disorders. The study found elevated injury risks across a wide spectrum of mental health conditions, reinforcing the idea that even common or moderate mental health challenges can have serious physical consequences over time.
This challenges the assumption that injury prevention should focus only on people with the most severe diagnoses. Instead, it suggests that mental health in general is an important factor in physical safety.
Why Mental Health May Increase Injury Risk
While the study focused on identifying risk rather than pinpointing exact causes, existing research offers several plausible explanations:
- Impaired concentration or attention, which can increase accident risk
- Slower reaction times, affecting driving or workplace safety
- Sleep disturbances, which are common in many mental health conditions
- Medication side effects, such as dizziness or fatigue
- Risk-taking behaviors, which may be more common during periods of psychological distress
These factors can combine to raise the likelihood of everyday accidents, especially over long periods.
Implications for Health Care and Policy
The findings carry important implications for both clinical care and public health policy.
Rethinking Mental Health Treatment
Researchers emphasize that mental health care should go beyond symptom management and include practical injury prevention strategies. This could involve:
- Educating patients about injury risks
- Addressing fall risk, driving safety, and workplace hazards
- Identifying opportunities to intervene during mental health-related hospital admissions
Improving Injury Surveillance
The study also highlights the need for better public health surveillance systems to track injuries among people with mental health conditions. Current systems often fail to connect mental health data with injury outcomes, leaving critical gaps in prevention efforts.
A More Integrated Health Care Model
Ultimately, the research supports a more integrated approach to health care, where mental and physical health are treated as deeply interconnected rather than separate domains.
Why This Research Is Especially Important
This study stands out not just for its size, but for its long follow-up period and cross-national design. By examining data from two different countries with robust health systems, the researchers strengthened confidence that the findings are not limited to a single health care system or cultural context.
It also shifts the conversation around mental health from a narrow focus on emotional well-being to a broader understanding of physical safety and long-term health outcomes.
What This Means for the Future
The findings suggest that people with mental health conditions represent an underrecognized population for injury prevention efforts. Addressing this gap could help reduce:
- Emergency room visits
- Long-term disability
- Health care costs
- Preventable deaths
Most importantly, it could improve quality of life for millions of people worldwide.
Mental health does not exist in isolation. This research makes it clear that protecting mental well-being also means protecting physical safety, and that the two should never be addressed separately.
Research Reference
Nature Mental Health (2025) – Mental health conditions are associated with increased risk of subsequent self-harm, assault and unintentional injuries in two nations
https://www.nature.com/articles/s44220-025-00553-w