Brain Scan Patterns Can Help Predict Recovery After Traumatic Brain Injury
Traumatic brain injury (TBI) is one of the most unpredictable conditions in modern medicine. Some patients regain their independence within months, while others are left with long-term or permanent disabilities. For doctors and families, one of the hardest challenges is knowing early on which path a patient is likely to take. A new large-scale neuroscience study suggests that specific patterns of brain activity, visible soon after injury, may help answer that question with far greater accuracy than current methods.
Researchers from Mass General Brigham, working alongside collaborators across the United States and Europe, have identified distinct neural connectivity patterns that are strongly associated with recovery six months after moderate to severe TBI. Their findings were published in the Proceedings of the National Academy of Sciences (PNAS) in 2025 and point toward a future where brain scans could play a central role in prognosis and decision-making after serious brain injury.
Why Predicting Recovery After TBI Is So Difficult
After a traumatic brain injury, especially a moderate or severe one, patients are often unconscious or dependent on life-sustaining therapies such as ventilators. Traditional neurological exams rely heavily on observable behavior, which may not be possible at this stage. Even advanced clinical scoring systems struggle to account for the complex and hidden damage occurring across brain networks.
This uncertainty makes it extremely difficult to predict long-term outcomes. Families are often forced to make critical decisions with limited information, and clinicians lack reliable tools to distinguish between patients who are likely to recover and those who are not.
Using Resting-State fMRI to Look Beneath the Surface
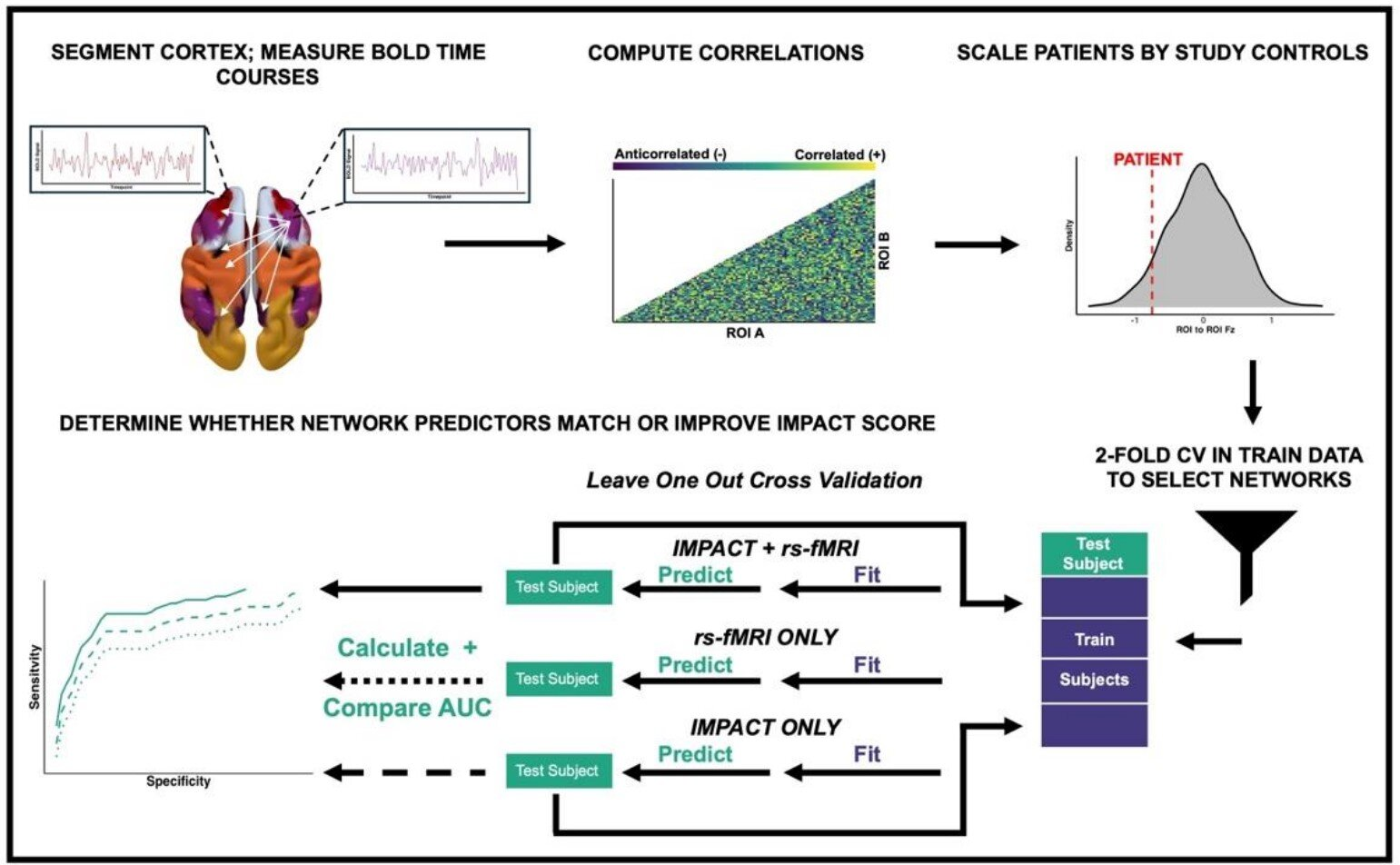
To tackle this problem, the research team turned to resting-state functional magnetic resonance imaging, commonly known as rs-fMRI. Unlike task-based MRI scans, rs-fMRI measures spontaneous brain activity while a person is at rest. This allows scientists to observe how different brain regions communicate with each other, even when the patient is unconscious or unable to follow instructions.
The study analyzed rs-fMRI data from 97 patients across three prospective cohorts, all of whom had suffered moderate to severe traumatic brain injuries. Brain scans were performed relatively early after injury, at a time when traditional prognosis is particularly uncertain.
The researchers then followed these patients for six months, assessing their functional outcomes using established clinical scales.
The Importance of Anticorrelated Brain Activity
One of the most important concepts explored in this study is anticorrelated brain activity. In a healthy brain, certain networks show an opposite pattern of activation: when one network becomes active, another becomes less active. This push-and-pull relationship is considered a hallmark of organized and efficient brain function.
After traumatic brain injury, these anticorrelations often weaken or disappear, reflecting disrupted communication between brain regions. The researchers wanted to know whether the preservation of these anticorrelated patterns early after injury could signal a better chance of recovery.
The answer, according to their data, was yes.
Three Key Connectivity Patterns Linked to Better Recovery
After analyzing the brain scans, the researchers identified three specific connectivity patterns that were strongly associated with favorable functional outcomes at six months. Patients who showed any one of these patterns were significantly more likely to recover, even after adjusting for factors such as sedation level and consciousness at the time of scanning.
First, the most powerful predictor involved connectivity between the salience network and the default mode network (DMN).
The salience network acts as a coordination hub, helping the brain decide which internal or external information deserves attention. The DMN, on the other hand, is most active during rest and internal thought. Healthy interaction between these two networks is believed to support conscious awareness and information integration.
Second, another beneficial pattern linked regions involved in cognitive control with areas responsible for basic visual processing. This suggests that preserved communication between higher-order thinking systems and sensory networks plays an important role in recovery.
Third, connectivity between the default mode network and the language network was also associated with better outcomes. This finding highlights the importance of language-related brain systems, even in patients who may not yet be able to speak or respond.
Building a Better Prediction Model
The researchers didn’t stop at identifying these patterns. They incorporated them into a predictive model designed to estimate recovery after traumatic brain injury. To ensure the model’s reliability, they used a rigorous validation approach, training it on one group of patients and testing it on another.
When compared to traditional prognostic models, the new brain-based approach performed significantly better at predicting six-month functional outcomes. Importantly, its accuracy held up across patients with different injury severities, across multiple hospitals, and even across MRI scanners in different countries.
This consistency suggests the findings are robust and not limited to a single clinical setting or imaging system.
Why These Findings Matter Clinically
The implications of this research are substantial. An objective, brain-based marker of recovery could dramatically improve early prognostic assessments after TBI. Instead of relying solely on behavioral signs or generalized scoring systems, clinicians could use direct evidence of preserved brain network function to guide discussions and decisions.
This could be especially valuable in intensive care units, where early prognostic uncertainty often influences treatment plans and long-term care strategies.
Could These Brain Networks Be Modified?
One of the most intriguing aspects of the study is the suggestion that these neural patterns may not just be markers of recovery, but potentially targets for future therapy. Previous research has shown that brain connectivity can be influenced by interventions such as neurostimulation, pharmacological treatments, and structured rehabilitation programs.
If future studies confirm that strengthening or restoring these specific networks improves outcomes, it could open the door to personalized, network-guided therapies for traumatic brain injury.
Understanding the Brain Networks Involved
To better appreciate the findings, it helps to understand the broader role of the networks identified in the study.
The default mode network is involved in self-referential thinking, memory, and baseline brain activity. Damage to this network has been linked to disorders of consciousness.
The salience network helps switch the brain between internal focus and external attention, making it crucial for awareness and responsiveness.
The frontoparietal cognitive control network supports decision-making and goal-directed behavior, while visual and language networks handle sensory input and communication.
The preservation of communication between these systems suggests that recovery from TBI is not dependent on a single brain region, but rather on the integrity of large-scale network interactions.
A Step Toward More Informed Decisions After TBI
While this research does not eliminate uncertainty, it represents a meaningful step toward more accurate and biologically grounded prognostic tools. Larger studies and longer follow-ups will be needed before this approach becomes routine in clinical practice. Still, the findings offer new hope for improving how recovery potential is assessed after traumatic brain injury.
By focusing on how the brain functions as a connected system, rather than isolated regions, this study reinforces a growing shift in neuroscience toward network-based understanding of brain health and recovery.
Research paper:
https://www.pnas.org/doi/10.1073/pnas.2518159122