Gene Therapy Switch Could Deliver Powerful Pain Relief Without the Risk of Addiction

A new preclinical study has revealed a promising gene therapy approach that could change how chronic pain is treated—by delivering strong pain relief without the addictive risks that come with opioid drugs. Developed by researchers at the University of Pennsylvania’s Perelman School of Medicine, in collaboration with teams from Penn Nursing, Carnegie Mellon University, and Stanford University, this work offers a highly targeted way to reduce pain by acting directly on specific brain circuits.
Chronic pain affects more than 50 million Americans, and for many, treatment options are limited to medications like morphine and other opioids. While these drugs can be effective, they often come with serious drawbacks, including tolerance, dependence, and addiction. The newly described gene therapy aims to separate pain relief from these harmful side effects by focusing only on the brain pathways that actually process pain.
A Precision Approach to Pain in the Brain
Traditional opioid medications work a bit like turning down the master volume on a stereo system. They reduce pain, but they also influence many other brain regions involved in reward, mood, breathing, and cognition. This broad effect is why opioids can cause euphoria, sedation, respiratory depression, and addiction.
The new gene therapy, by contrast, is designed to work more like a dedicated volume knob for pain alone. Researchers identified specific neural circuits in the brain—particularly within cortical pain centers—that are responsible for encoding the emotional and motivational aspects of pain. These are the same circuits that opioids like morphine act on to reduce suffering.
By targeting only these pain-related circuits, the therapy reduces pain signals while leaving other brain functions untouched. In preclinical models, this approach provided strong and durable pain relief without activating reward pathways, meaning it did not produce behaviors associated with addiction.
Using AI to Measure Pain More Accurately
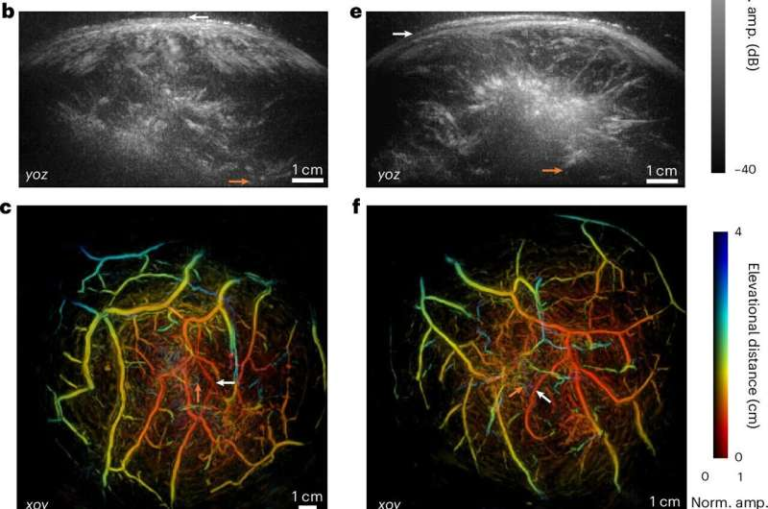
One of the most innovative aspects of the study is how the researchers measured pain. Pain is notoriously difficult to quantify, especially in animal models. To address this, the team developed an AI-driven behavioral platform that tracks natural mouse behaviors with high precision.
This system analyzes movement patterns, posture, and other subtle behaviors to create an objective “pain readout.” Instead of relying on single reflex-based tests, the AI provides a more comprehensive picture of how much pain an animal is experiencing in daily life. This allowed researchers to determine how much intervention was needed to meaningfully reduce pain—and to confirm that the therapy was working as intended.
The AI-generated data served as a blueprint for designing the gene therapy itself, ensuring it closely mimicked the beneficial effects of opioids while avoiding their harmful consequences.
How the Gene Therapy Works
The therapy uses a central nervous system–targeted gene delivery strategy, widely believed to be the first of its kind specifically designed for pain. Using viral vectors, the researchers delivered genetic instructions directly to pain-processing neurons in the brain.
Once delivered, these instructions act as a molecular “off switch” for pain. When activated, the switch dampens activity in pain-related circuits, leading to long-lasting relief. Importantly, this intervention does not interfere with normal sensation, movement, or reward-related brain activity.
In animal studies, the therapy produced pain relief comparable to morphine—but without tolerance. The animals did not require increasing doses over time, and they did not display behaviors linked to drug-seeking or addiction.
Why Avoiding Addiction Matters So Much
The timing of this research is especially important given the ongoing opioid crisis. In 2019 alone, around 600,000 deaths in the United States were attributed to drug use, with approximately 80% linked to opioids. Surveys show that nearly half of people in cities like Philadelphia know someone with opioid use disorder, and a significant number know someone who has died from an overdose.
At the same time, chronic pain is often described as a silent epidemic, costing hundreds of billions of dollars each year in direct medical expenses and lost productivity. Many patients face an impossible choice: live with debilitating pain or risk addiction through long-term opioid use.
This gene therapy approach aims to ease one crisis without fueling another.
Years of Research Behind the Discovery
The findings are the result of more than six years of research into how chronic pain is encoded in the brain. By carefully mapping the neural circuits involved, the researchers were able to pinpoint exactly where opioids exert their pain-relieving effects—and where addiction-related effects begin.
This detailed understanding made it possible to design a therapy that separates the two. The study provides what the researchers describe as a concrete blueprint for non-addictive, circuit-specific pain medicine.
What Comes Next
It is important to note that this work is still in the preclinical stage. All experiments were conducted in animal models, and significant testing remains before the therapy can be evaluated in humans. Safety, long-term effects, delivery methods, and regulatory approval are all challenges that lie ahead.
The research team is now moving into the next phase of work, with the goal of bridging the gap between discovery and future clinical trials. While the journey from lab to clinic is long, the results so far represent a strong and encouraging first step.
How This Fits Into the Bigger Picture of Pain Medicine
Pain research has increasingly shifted toward precision medicine, where treatments are tailored to specific biological mechanisms rather than applied broadly. This gene therapy fits squarely within that trend.
Instead of flooding the entire nervous system with drugs, circuit-specific therapies aim to correct dysfunctional signaling at its source. If successful in humans, this approach could open the door not only to safer pain treatments but also to new therapies for other neurological and psychiatric conditions where specific brain circuits are involved.
Gene therapy itself has made major advances in recent years, with improved targeting, better safety profiles, and growing regulatory acceptance. The idea of using it to treat pain—long considered too complex and subjective—marks a significant shift in how researchers think about managing chronic suffering.
A Potential Turning Point for Chronic Pain Treatment
While much work remains, this study offers real hope for a future where people with chronic pain are no longer forced to choose between relief and addiction. By combining neuroscience, artificial intelligence, and gene therapy, the researchers have demonstrated that it may be possible to deliver powerful pain relief in a far safer way.
If these findings translate successfully to humans, they could represent a major turning point in pain medicine—one that reduces suffering while helping to stem the tide of opioid misuse.
Research paper: https://www.nature.com/articles/s41586-025-09908-w