More Than a Quarter of Adults Worldwide Could Benefit From GLP-1 Medications for Weight Loss, Major Global Study Finds

The global obesity crisis has been quietly accelerating for decades, and a new large-scale study now puts a striking number on just how many people could potentially benefit from modern medical treatment. According to new research led by Mass General Brigham, more than one in four adults worldwide may be eligible for GLP-1 receptor agonist medications for weight management. These findings add fresh urgency to ongoing conversations about obesity, health equity, and access to life-changing medications.
Obesity Has More Than Doubled Worldwide
Over the last 30 years, the worldwide prevalence of obesity has more than doubled, affecting nearly every region and income group. This surge has gone hand in hand with rising rates of type 2 diabetes, cardiovascular disease, hypertension, and certain cancers. Beyond individual health impacts, obesity places enormous strain on healthcare systems, public budgets, and national economies.
While lifestyle changes like diet and physical activity remain important, researchers increasingly recognize that obesity is driven by complex biological mechanisms, not just personal choices. This growing understanding has pushed scientists and policymakers to explore medical tools that can complement traditional prevention strategies.
A Massive Global Dataset
To better understand how many people might benefit from GLP-1 medications, researchers from Mass General Brigham, Washington University School of Medicine in St. Louis, and Emory University’s Rollins School of Public Health conducted one of the largest analyses of its kind.
The team pooled household health survey data from 99 countries, collected between 2008 and 2021. The final dataset included 810,635 adults between the ages of 25 and 64. Importantly, the researchers only included participants with reliable measurements for body mass index (BMI), blood pressure, diabetes biomarkers, and documented histories of hypertension or diabetes.
This rigorous approach allowed the team to apply widely accepted clinical eligibility criteria for GLP-1 medications on a truly global scale.
Who Was Considered Eligible?
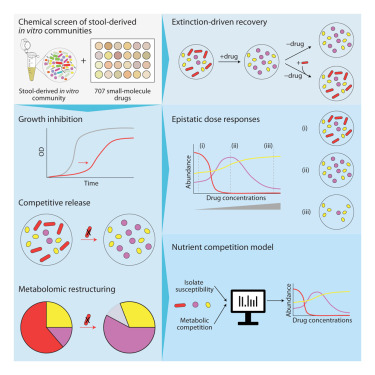
Eligibility for GLP-1 medications in the study followed standard medical guidelines. Adults were considered eligible if they met either of the following criteria:
- A BMI greater than 30, which falls into the obesity category
- A BMI greater than 27 combined with hypertension, type 2 diabetes, or both
Using these benchmarks, researchers found that 27% of adults worldwide met eligibility requirements for GLP-1 medications for weight management.
The Global Picture Is Uneven
One of the most striking findings is where eligible individuals are located. Roughly four-fifths of adults eligible for GLP-1 medications live in low- and middle-income countries, highlighting a major challenge for global access and affordability.
Eligibility rates varied widely by region:
- Europe and North America showed the highest eligibility rate at 42.8%
- The Pacific Islands followed closely at 41.0%
- Other regions showed lower but still significant proportions of eligible adults
These patterns reflect differences in diet, urbanization, economic development, and access to healthcare, but they also raise serious questions about how these medications can be made available in places with fewer resources.
Women and Older Adults Stand Out
The study also revealed important gender and age differences. Women were more likely to be eligible for GLP-1 medications than men, with 28.5% meeting eligibility criteria. Age played an even stronger role: older adults had much higher eligibility rates (38.3%) compared with younger adults (17.9%).
These differences matter because obesity-related diseases often have more severe consequences later in life and disproportionately affect women in certain regions. In some countries, type 2 diabetes has become one of the leading causes of death among women, underscoring the potential impact of targeted treatment strategies.
Why GLP-1 Medications Are Different
GLP-1 receptor agonists have transformed how clinicians think about obesity. Originally developed to treat type 2 diabetes, these medications work by mimicking a natural hormone that regulates appetite, satiety, and blood sugar levels. Patients typically experience reduced hunger, slower gastric emptying, and improved metabolic control.
Unlike older weight-loss drugs, GLP-1 medications address the biological drivers of weight gain, not just behavior. This shift has helped challenge the long-held idea that obesity is simply a failure of willpower.
Recognition From the World Health Organization
The promise of GLP-1 medications has not gone unnoticed. The World Health Organization (WHO) is actively working to evaluate how these drugs could be incorporated into global obesity treatment guidelines. WHO officials have emphasized that obesity is a chronic, relapsing condition that often requires long-term management, much like diabetes or hypertension.
However, WHO has also stressed that medications should be used alongside lifestyle interventions, not as a replacement for them. Diet, physical activity, and preventive public health measures remain essential components of obesity control.
Major Barriers Remain
Despite their potential, GLP-1 medications face significant hurdles. Cost, limited supply, and health system capacity remain major barriers, particularly in low-resource settings. Even in high-income countries, access is often restricted by insurance coverage, prescribing rules, and long waiting lists.
Researchers involved in the study caution that further work is needed to understand the long-term safety, sustainability, and population-level impact of widespread GLP-1 use. At the same time, they emphasize that investment in non-pharmacological prevention strategies remains critically underfunded worldwide.
Why These Findings Matter
This study provides one of the clearest global estimates to date of how many adults could benefit from GLP-1 medications. By quantifying eligibility across regions, income levels, genders, and age groups, the research offers valuable data for policymakers, public health planners, and healthcare systems preparing for the next phase of obesity treatment.
At its core, the message is simple but powerful: obesity is a global health challenge driven by biology, environment, and inequality. GLP-1 medications are not a silver bullet, but they represent one of the most promising tools yet for reducing the burden of obesity and its related diseases—if access can be made fair and sustainable.
Research paper: https://doi.org/10.1016/S2213-8587(25)00356-0