New Brain Study Explains How Binge Drinking Leads to Long-Lasting Negative Feelings
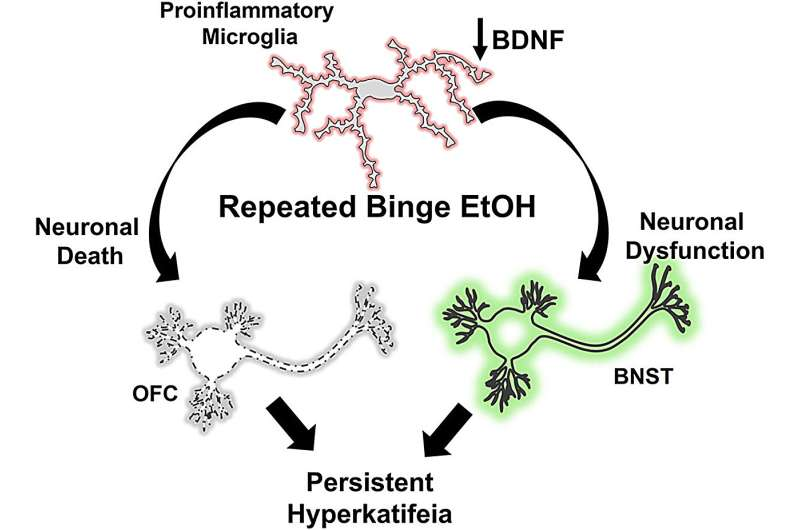
A new brain study has taken a deeper look at why repeated binge drinking can leave people feeling emotionally low long after the alcohol is gone. The research points to neuroinflammation, driven by the brain’s immune cells called microglia, as a key biological mechanism behind prolonged negative emotional states linked to heavy alcohol use. These findings help explain why binge drinking doesn’t just affect the body temporarily but can reshape emotional health in lasting ways.
The study, published in The American Journal of Pathology, focuses on a condition known as hyperkatifeia, a term used to describe an intense and persistent state of negative emotions such as anxiety, irritability, and emotional distress. Hyperkatifeia is increasingly recognized as a major factor that fuels alcohol use disorder (AUD) and increases the risk of relapse, even after someone stops drinking.
Understanding the Emotional Toll of Repeated Binge Drinking
Alcohol use disorder often develops through a cycle that combines life stress, binge drinking, withdrawal, and emotional distress. Stressful life events can trigger alcohol use, and repeated binge drinking episodes then create additional stress within the brain itself. Over time, these cycles interact and intensify, producing persistent negative emotions that make it harder for individuals to quit drinking.
The researchers behind this study were interested in understanding whether microglia, the immune cells responsible for maintaining brain health, directly contribute to these long-lasting emotional changes. Previous research had already shown that neuroinflammation is common in people with AUD, but it was unclear whether microglia were actively driving emotional disturbances or merely responding to damage caused by alcohol.
Because neuroinflammation is known to influence mood and behavior in other conditions, the researchers suspected that microglia might play a more central role in shaping alcohol-related emotional changes than previously thought.
How the Study Was Conducted
To explore this question, researchers used mouse models to simulate patterns of binge drinking and withdrawal. The mice were divided into groups that received either short-term binge alcohol exposure lasting four days or longer-term exposure lasting ten days. After the alcohol exposure ended, the mice were evaluated during periods of abstinence.
The scientists assessed anxiety-like behavior, fear memory, and signs of neuronal damage in the brain. In another set of experiments, microglia were selectively inhibited using a targeted genetic technique during alcohol exposure. This allowed the researchers to directly test whether preventing microglial activation would change emotional outcomes and brain health.
Key Findings From the Research
The results showed a clear difference between short-term and prolonged binge drinking. Mice exposed to alcohol for ten days, but not four days, developed brain damage and persistent negative emotional states. This longer exposure activated microglia, triggering long-lasting neuroinflammation that continued even after alcohol use stopped.
When microglial activation was blocked during the ten-day binge period, the results were striking. Preventing pro-inflammatory microglia activity stopped alcohol-induced neuronal death and prevented anxiety-like behavior during withdrawal. It also blocked the formation of persistent fear memories during abstinence, which are believed to contribute to ongoing emotional distress.
These findings strongly suggest that microglia are not just passive bystanders but active drivers of emotional and neurological damage associated with repeated binge drinking.
Why Microglia Matter in Alcohol-Related Brain Changes
Microglia play an essential role in maintaining brain health. Under normal conditions, they help remove damaged cells, support neurons, and regulate immune responses. However, repeated heavy alcohol exposure can push microglia into a pro-inflammatory state.
Once activated in this way, microglia release inflammatory molecules that can disrupt neural signaling, damage neurons, and alter brain circuits involved in emotion and stress. The study found evidence of damage in brain regions involved in emotional regulation, including areas linked to fear, anxiety, and decision-making.
This inflammatory response appears to create a vicious cycle. Alcohol activates microglia, inflammation damages emotional circuits, negative feelings intensify, and individuals may drink again to escape those feelings. Over time, this cycle becomes increasingly difficult to break.
The Link Between Negative Emotions and Alcohol Use Disorder
Negative emotional states caused by alcohol play a significant role in the development and persistence of AUD. Hyperkatifeia not only increases the desire to drink but is also linked to depression, anxiety disorders, and other mental health conditions.
Globally, nearly 95 million people are affected by alcohol use disorder. While treatments exist, including medications like naltrexone, acamprosate, and disulfiram, along with behavioral therapies and support groups, outcomes remain challenging. Around 60 percent of individuals relapse within the first year after treatment.
One major reason for this high relapse rate is that current treatments do not specifically target alcohol-induced negative emotional states. This study highlights a biological mechanism that could explain why emotional distress lingers even after drinking stops.
New Possibilities for Treatment
One of the most important implications of this research is the potential for immune-based therapies to treat alcohol-related mood disturbances. By targeting microglia and reducing neuroinflammation, it may be possible to interrupt the cycle of negative emotions that drives continued alcohol use.
The researchers noted that the level of protection achieved by inhibiting microglia was unexpectedly strong. Blocking microglial activation not only preserved neuronal health but also prevented the emotional symptoms that typically follow repeated binge drinking.
This opens the door to developing medications that specifically address hyperkatifeia, something no current AUD treatment is designed to do.
Broader Context: Alcohol, Inflammation, and the Brain
Alcohol’s impact on the brain goes beyond intoxication and hangovers. Chronic and repeated binge drinking has long been associated with neurodegeneration, disrupted neurotransmitter systems, and changes in brain structure. Neuroinflammation is increasingly recognized as a unifying factor behind many of these effects.
Repeated cycles of alcohol use and withdrawal can sensitize the brain, making it more reactive to stress and inflammation. This phenomenon helps explain why emotional symptoms often worsen over time with continued heavy drinking, even if consumption levels stay the same.
Understanding the role of microglia provides a clearer biological explanation for these changes and reinforces the importance of avoiding sustained binge drinking patterns.
What This Study Adds to Our Understanding
This research is significant because it demonstrates a causal link between microglial activation and long-lasting emotional damage caused by binge alcohol exposure. Rather than simply observing inflammation alongside emotional symptoms, the study shows that stopping microglial activation can prevent both brain damage and negative emotions.
These findings highlight that the emotional consequences of binge drinking are not just psychological or behavioral but deeply rooted in brain biology. They also underscore the importance of early intervention and prevention, especially for individuals who engage in repeated binge drinking.
Research Reference
Microglia Promote Neurodegeneration and Hyperkatifeia during Withdrawal and Abstinence from Binge Alcohol
The American Journal of Pathology (2026)
https://doi.org/10.1016/j.ajpath.2025.10.005