Neurologists Use AI to Close Diagnostic Gaps in Seizure Care
Neurologists and clinician-scientists at the University of Pittsburgh School of Medicine have developed a new artificial intelligence–based diagnostic tool that could meaningfully improve how seizures are diagnosed, especially in cases that are often misunderstood or missed. The research focuses on functional seizures, a condition frequently mistaken for epilepsy, and shows how AI can help clinicians make more accurate decisions, reduce unnecessary treatments, and improve patient safety.
The study, published in the medical journal Epilepsia, highlights a persistent challenge in seizure care: distinguishing between epileptic seizures and functional seizures. While both can look similar on the surface, their causes and treatments are very different. The researchers demonstrate that AI can act as a powerful support system for clinicians, particularly those without specialized neurology training, by identifying cases that deserve closer review.
Functional seizures account for around 10% of all seizure cases, yet they are commonly misdiagnosed. Unlike epileptic seizures, which are caused by abnormal electrical activity in the brain, functional seizures arise from a complex mix of biological, psychological, and social factors. Because there is no abnormal electrical signal driving these events, standard antiseizure medications do not work. When misdiagnosis occurs, patients may spend years on ineffective medications while the real underlying issue remains untreated.
The research team was led by Dr. Wesley T. Kerr, an assistant professor of neurology and bioinformatics at the University of Pittsburgh and lead epileptologist of the UPMC Functional Neurological Disorders Program. His work focuses on closing diagnostic gaps that leave many patients without the right care. According to Kerr, clinicians are trained to assume seizures are epileptic because most of them are. The problem is that the remaining cases—those that are not epilepsy—represent a critical blind spot in modern neurology.
The AI tool developed by Kerr and his colleagues was designed to address exactly this issue. Rather than replacing clinicians, the system provides an additional checkpoint, encouraging healthcare providers to consider functional seizures when the clinical picture does not fully align with epilepsy. The idea is not to override human judgment, but to expand it.
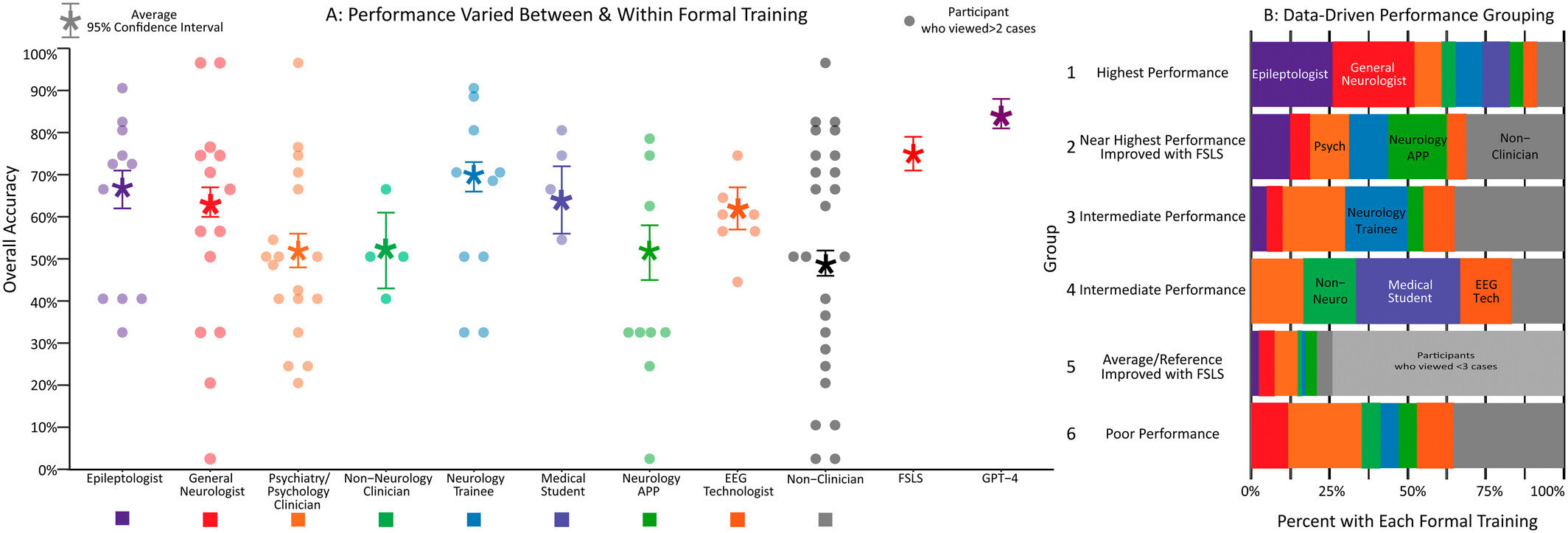
To test how well the AI tool worked, the researchers designed a large and carefully controlled study. They presented 117 anonymized patient cases to 163 reviewers from a wide range of backgrounds. Participants included non-clinicians, medical students, non-neurology physicians, technologists, advanced practice providers, neurologists, and expert epileptologists. Each reviewer evaluated a randomized subset of cases and made diagnostic decisions both before and after receiving AI assistance.
The results were striking. Overall, 66% of reviewers showed improved diagnostic accuracy after using the AI tool. Among average clinicians and those comfortable working with AI systems, accuracy in identifying functional seizures improved by nearly 20%. This improvement was particularly important for clinicians who do not specialize in neurology, as they are often the first point of contact for patients experiencing seizures.
Interestingly, the AI tool did not significantly improve performance among expert epileptologists. This was not seen as a failure of the system. Instead, it demonstrated that the AI’s recommendations closely mirrored the knowledge and reasoning already used by specialists. In other words, the tool performed at an expert level, making it especially valuable in settings where experts are not available.
One of the key goals of this research is to reduce unnecessary treatments. Patients with functional seizures are often prescribed antiseizure medications that do nothing to address the root cause of their condition. These medications can carry serious side effects, particularly for pregnant patients, older adults, and people with complex medical conditions. By helping clinicians recognize functional seizures earlier, the AI tool could limit exposure to medications that offer no benefit and may even cause harm.
Functional seizures are often described as a form of “panic without panic.” The body enters a state of extreme stress response, but the individual may not consciously experience fear or anxiety. Instead, the stress manifests physically as a seizure. Treatment focuses on neurobehavioral therapy, education, and addressing underlying stressors rather than medication. Getting the diagnosis right is therefore essential, as the treatment pathways for epilepsy and functional seizures are completely different.
Beyond improving diagnosis in clinical settings, the research team is already looking ahead. One of the next steps involves exploring AI-assisted analysis of seizure videos. Currently, the gold standard for confirming whether a seizure is epileptic or functional is inpatient video-EEG monitoring, which requires hospitalization and significant resources. AI-based video analysis could potentially reduce the need for inpatient monitoring, making diagnosis faster, less invasive, and more accessible.
Another major goal is integrating the AI tool directly into electronic health records. In this model, the system would automatically analyze patient data and flag cases where functional seizures should be considered. Clinicians would still make the final decision, but the AI would ensure that fewer cases slip through the cracks.
Why Functional Seizures Are So Hard to Diagnose
Functional seizures sit at the intersection of neurology, psychology, and social health, which makes them particularly challenging. They do not show the clear EEG markers associated with epilepsy, and symptoms can vary widely between patients. Many people with functional seizures also experience stigma, delayed diagnosis, and frustration after years of ineffective treatment.
Historically, these seizures were poorly understood and sometimes dismissed as “not real,” a misconception that still affects patient care today. Modern research emphasizes that functional seizures are very real medical events, even though their mechanism differs from epilepsy. Tools like the one developed at Pitt could help shift clinical culture toward earlier recognition and more compassionate care.
The Growing Role of AI in Neurology
This study also fits into a broader trend of AI adoption in neurology and medicine. AI systems are increasingly used for EEG interpretation, imaging analysis, risk prediction, and clinical decision support. What makes this work stand out is its focus on equity in care—bringing expert-level insights to clinicians and patients who might otherwise lack access to specialized neurology services.
The researchers stress the importance of ethical oversight and transparency as AI tools become more common in healthcare. The goal is not automation for its own sake, but better outcomes for patients through smarter, more informed decision-making.
As AI continues to evolve, tools like this one may help ensure that fewer patients are misdiagnosed, fewer unnecessary medications are prescribed, and more people receive care that truly matches their condition. In seizure medicine, where the cost of diagnostic errors can be high, that shift could make a lasting difference.
Research paper: https://doi.org/10.1002/epi.70069