Near-Atomic Imaging Reveals a Promising New Target for the ‘Brain on Fire’ Autoimmune Disease

Scientists have uncovered an important new clue in the fight against a devastating autoimmune brain disorder often referred to as the “Brain on Fire” condition, formally known as anti-NMDA receptor encephalitis. Using cutting-edge imaging technology, researchers at Oregon Health & Science University (OHSU) have identified specific regions on a key brain receptor that could become targets for more precise treatments and even earlier diagnosis of the disease.
This discovery offers fresh hope for patients affected by a condition that can rapidly disrupt memory, behavior, and basic brain function, and which is still frequently misdiagnosed in its early stages.
What Is the ‘Brain on Fire’ Condition?
Anti-NMDA receptor encephalitis is a rare but severe autoimmune disease in which the body’s immune system mistakenly attacks the brain. The primary target of this attack is the NMDA receptor, a crucial protein involved in communication between neurons. These receptors play a central role in learning, memory, and cognition, so interference with their function can have profound effects.
The condition gained public attention through the bestselling memoir and later the 2016 film “Brain on Fire,” which chronicled a young woman’s struggle with the disease. Despite increased awareness, it remains rare, affecting roughly 1 in 1 million people each year, most commonly young adults in their 20s and 30s.
Symptoms can begin subtly, often with psychiatric changes, confusion, anxiety, or hallucinations. As the disease progresses, patients may experience severe memory loss, seizures, loss of speech, abnormal movements, and even death if not treated promptly.
The Autoimmune Attack on NMDA Receptors
At the heart of the disease are autoantibodies—immune proteins that mistakenly bind to and disrupt the brain’s NMDA receptors. These autoantibodies specifically target parts of the receptor, interfering with its normal function and triggering widespread neurological symptoms.
While researchers have known for years that NMDA receptors are involved, pinpointing exactly where and how the antibodies bind has been a major challenge. That is where the new OHSU study makes a critical advance.
Near-Atomic Imaging Sheds New Light
In the new research, scientists used near-atomic resolution cryo-electron microscopy (cryo-EM) to visualize the NMDA receptor in extraordinary detail. This advanced imaging technique allows researchers to see biological structures at a level close to individual atoms, revealing interactions that were previously invisible.
The work was conducted at the Pacific Northwest Cryo-EM Center, located on OHSU’s South Waterfront campus. This facility is one of only three national centers equipped with this state-of-the-art imaging technology.
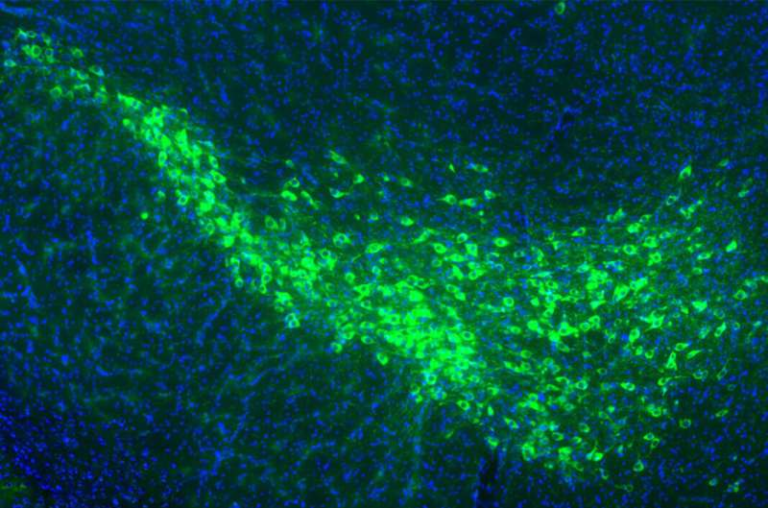
By applying cryo-EM, the research team was able to map precise antibody binding sites on the NMDA receptor, identifying what they describe as antigenic hot spots—specific regions that attract the harmful autoantibodies.
Mouse Models and Human Evidence Align
A key strength of the study is how closely the experimental findings matched real-world patient data. The research team analyzed autoantibodies collected from a specially engineered mouse model of anti-NMDA receptor encephalitis. This mouse model had been developed earlier by OHSU researchers to closely mimic the human disease.
Lead author Junhoe Kim, Ph.D., a postdoctoral fellow at the OHSU Vollum Institute, compared the antibody binding patterns from these mice with autoantibodies isolated from people diagnosed with the disease. Remarkably, the binding sites in the mouse model overlapped almost perfectly with those seen in human patients.
This alignment provides strong evidence that the mouse model accurately reflects the human condition and that the identified binding regions are truly relevant to patient disease.
A Single, Targetable Hot Spot
One of the most exciting aspects of the discovery is that nearly all of the disease-associated antibodies clustered around a single domain on a subunit of the NMDA receptor. This particular region is structurally simpler than other parts of the receptor, making it far easier to target with drugs.
Instead of needing to suppress the entire immune system, future therapies could potentially focus on blocking this specific antibody–receptor interaction, preserving normal immune function while stopping the disease process at its source.
Why Current Treatments Fall Short
At present, treatment for anti-NMDA receptor encephalitis relies largely on broad immunosuppression. Patients are typically treated with steroids, intravenous immunoglobulin (IVIG), plasma exchange, or more aggressive immune-modulating drugs.
While many patients do improve, these treatments do not always work, and relapses are common. Broad immunosuppression can also leave patients vulnerable to infections and other complications.
Neurologist and co-author Gary Westbrook, M.D., emphasized that the new findings highlight the need for more precise therapeutic approaches that go beyond the blunt tools currently available.
New Possibilities for Diagnosis
Beyond treatment, the study also opens the door to improved diagnostics. Because the researchers now know the exact regions of the NMDA receptor that autoantibodies target, it may be possible to develop a blood-based test that detects these antibodies earlier in the disease process.
Earlier diagnosis is especially important because many patients initially present with psychiatric symptoms and are misdiagnosed, delaying proper treatment. A reliable blood test could significantly reduce these delays and improve outcomes.
The Researchers Behind the Discovery
The study was led by scientists at OHSU’s Vollum Institute, with senior author Eric Gouaux, Ph.D., a Howard Hughes Medical Institute investigator, playing a central role. Additional co-authors included Farzad Jalali-Yazdi, Ph.D., and Brian Jones, Ph.D., also of OHSU.
The collaborative effort combined expertise in neuroscience, immunology, structural biology, and advanced imaging technology.
A Broader Look at NMDA Receptors
NMDA receptors are essential for synaptic plasticity, the process by which the brain strengthens or weakens connections between neurons. This plasticity underlies learning and memory, which helps explain why disrupting these receptors leads to such profound cognitive and behavioral symptoms.
Because NMDA receptors are so central to brain function, any therapy targeting them must be highly specific. The newly identified antibody hot spots provide exactly that kind of specificity, making this discovery especially valuable.
Why This Discovery Matters
This research represents a major step forward in understanding anti-NMDA receptor encephalitis at a molecular level. By revealing exactly where harmful antibodies bind, scientists now have a clear roadmap for developing targeted therapies and better diagnostic tools.
While new treatments will still take time to develop and test, this work lays the foundation for safer, more effective, and more precise interventions that could dramatically improve the lives of patients affected by this rare but devastating disease.
Research paper:
Cryo-EM of autoantibody-bound NMDA receptors reveals antigenic hot spots in an active immunization model of anti-NMDAR encephalitis, Science Advances (2026)
https://www.science.org/doi/10.1126/sciadv.aeb4249