The Stop-Smoking Medication Varenicline May Also Help Treat Cannabis Use Disorder
A medication that has long been used to help people quit smoking cigarettes may also have potential in treating cannabis use disorder (CUD)—at least for some people. A newly published randomized controlled trial suggests that varenicline, best known under the brand names Chantix and Champix, can help reduce cannabis use in men diagnosed with CUD, while showing no clear benefit for women. The findings add an important new piece to a field where effective medications are still largely missing.
Understanding Cannabis Use Disorder and Why It Matters
Cannabis use disorder is defined by continued cannabis use despite clear negative consequences. These consequences can include problems at work or school, strained relationships, neglect of responsibilities, and ongoing use even when cannabis contributes to physical or psychological issues. Clinically, CUD is also associated with withdrawal symptoms, sleep disturbances, anxiety, mood disorders, and an increased risk of psychosis, particularly in vulnerable individuals.
The condition is becoming more common worldwide. One major reason is changing cannabis laws, with legalization and decriminalization expanding access in several countries and many U.S. states. While legalization does not automatically lead to addiction, broader availability does increase the number of people at risk. Despite this growing public health issue, there are currently no FDA-approved medications specifically for treating cannabis use disorder. Most treatment approaches rely on behavioral therapies, counseling, and psychosocial support.
That gap is what makes this new study especially interesting.
Why Researchers Looked at Varenicline
Varenicline is a well-established smoking cessation medication. It works by partially stimulating nicotinic acetylcholine receptors in the brain—the same receptors nicotine acts on—while also blocking nicotine’s full rewarding effects. This dual action helps reduce cravings and withdrawal symptoms while making smoking less satisfying.
Researchers have long suspected that nicotine and cannabis share overlapping brain reward pathways, particularly those involving dopamine. Because of this overlap, scientists wondered whether a medication effective for tobacco dependence might also influence cannabis use. Earlier, smaller studies hinted at this possibility, but strong clinical evidence was lacking.
The new trial was designed to directly test whether varenicline could reduce cannabis use in people diagnosed with cannabis use disorder.
How the Study Was Designed
The trial was conducted at the Medical University of South Carolina and published in the peer-reviewed journal Addiction. It followed a double-blind, randomized, placebo-controlled design, which is considered the gold standard for clinical research.
A total of 174 adults with cannabis use disorder took part. To qualify, participants had to report using cannabis at least three days per week. They were randomly assigned to receive either:
- Varenicline, gradually increased to a target dose of 1 mg twice daily, or
- A placebo pill designed to look identical
The treatment period lasted 12 weeks. Importantly, all participants—regardless of which medication they received—also took part in weekly brief medical management sessions. These sessions focused on encouraging medication adherence and supporting participants in following the study protocol, but they were not intensive psychotherapy.
The primary outcome researchers focused on was the number of self-reported cannabis use sessions per week, particularly during weeks 6 through 12 of the trial. Participants were also followed for one week after treatment ended to see whether any effects persisted.
The Key Finding: Sex Differences Matter
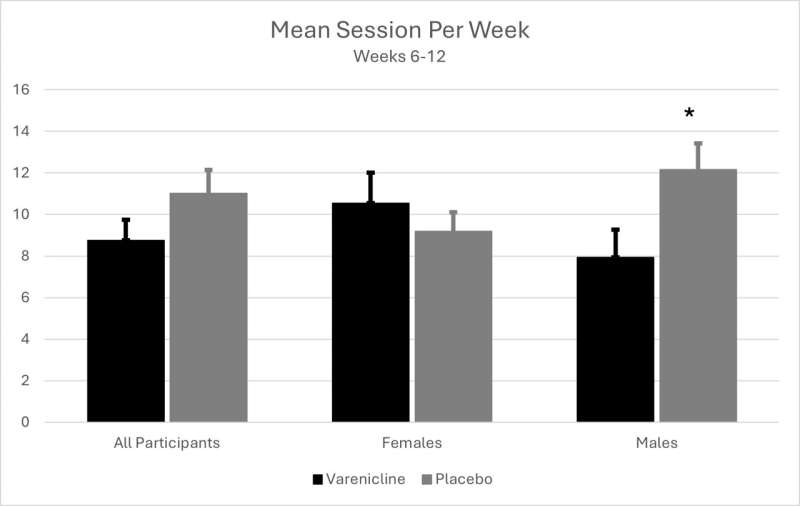
When researchers looked at the entire group of participants together, varenicline did not significantly outperform placebo. However, when the data were analyzed by sex, a clear and important difference emerged.
Results in Men
Men who received varenicline showed a meaningful reduction in cannabis use compared with men who received placebo. On average:
- Men in the varenicline group reported about 7.9 cannabis use sessions per week during the treatment period
- Men in the placebo group reported more than 12 sessions per week
- In the week after treatment ended, men who had taken varenicline reduced their use further, averaging 5.7 sessions per week
In addition to fewer sessions, men on varenicline also used cannabis on fewer days per week—about 3.8 days, compared with 4.7 days in the placebo group. These differences were statistically significant, suggesting that the medication had a real effect rather than a chance result.
Results in Women
For women, the picture was very different. Women who received varenicline did not reduce their cannabis use compared with those on placebo. In fact:
- Women on varenicline averaged just over 10 sessions per week
- Women on placebo averaged about 9.2 sessions per week, dropping to 8.2 sessions in the week after treatment
Women taking varenicline also reported higher levels of withdrawal symptoms, stronger cravings, and increased anxiety compared with other groups in the study. These effects may help explain another important finding: women on varenicline had lower medication adherence than women taking placebo. In other words, they were less likely to take the medication as prescribed.
Why Might Men and Women Respond Differently?
The study was not designed to fully explain why these sex differences occurred, but several possibilities exist. Biological differences in hormones, brain chemistry, and receptor sensitivity could influence how varenicline interacts with the nervous system. Psychological and social factors may also play a role, including how men and women experience withdrawal or side effects.
Interestingly, varenicline works equally well for men and women when used to treat nicotine dependence, which makes the cannabis-specific difference even more intriguing. The authors emphasize that these findings highlight the importance of sex-specific research rather than assuming one-size-fits-all treatments.
Why This Study Is Important
Cannabis use disorder is rising quickly, yet treatment options remain limited. This trial is one of the first well-controlled studies to show that a medication can reduce cannabis use in a specific subgroup of patients. While varenicline is clearly not a universal solution, it may become a useful option for men with CUD, especially if combined with behavioral therapies.
At the same time, the lack of benefit—and possible worsening of symptoms—in women underscores the need for more targeted research. The researchers plan to conduct future studies with larger samples of women to better understand these effects and explore whether different dosing strategies or additional supports might change outcomes.
A Broader Look at Medications for Cannabis Use Disorder
Over the years, researchers have tested a wide range of medications for CUD, including antidepressants, mood stabilizers, cannabinoid-based treatments, and medications used for other substance use disorders. So far, none have consistently demonstrated strong effectiveness, which is why behavioral therapies remain the primary treatment.
The varenicline findings add cautious optimism. They suggest that repurposing existing medications—especially those that act on shared brain pathways—could be a productive direction for future research.
What Comes Next
For now, varenicline is not approved specifically for cannabis use disorder, and people should not use it for this purpose without medical supervision. Still, the study opens the door to new conversations about pharmacological treatments for CUD and highlights how critical it is to consider sex differences in addiction research.
As cannabis use continues to rise globally, even partial solutions could make a meaningful difference for many people.
Research paper:
https://doi.org/10.1111/add.70296