More Than Just Fear A New Scientific Profile of Post-Traumatic Stress Disorder

Post-traumatic stress disorder, commonly known as PTSD, has long been understood through a fairly narrow lens. Popular culture, clinical models, and even many treatment approaches tend to focus on fear-based symptoms—flashbacks, nightmares, hypervigilance, and exaggerated startle responses. But new research from Yale School of Medicine suggests this picture is incomplete. According to a recent study, PTSD is not driven by fear alone. Instead, it appears to involve two distinct emotional profiles, one rooted in fear and another centered on emotional pain.
This emerging perspective could have major implications for how PTSD is diagnosed, studied, and treated.
Rethinking What PTSD Really Looks Like
PTSD is known to be a highly complex and varied condition. People exposed to trauma can experience symptoms in very different ways, even if they meet the same diagnostic criteria. Despite this diversity, most clinical frameworks have historically emphasized fear as the primary driver of PTSD symptoms.
Researchers involved in this study questioned that assumption. They proposed that fear captures only part of the PTSD experience and that another emotional force—emotional pain—may play an equally important role for many individuals.
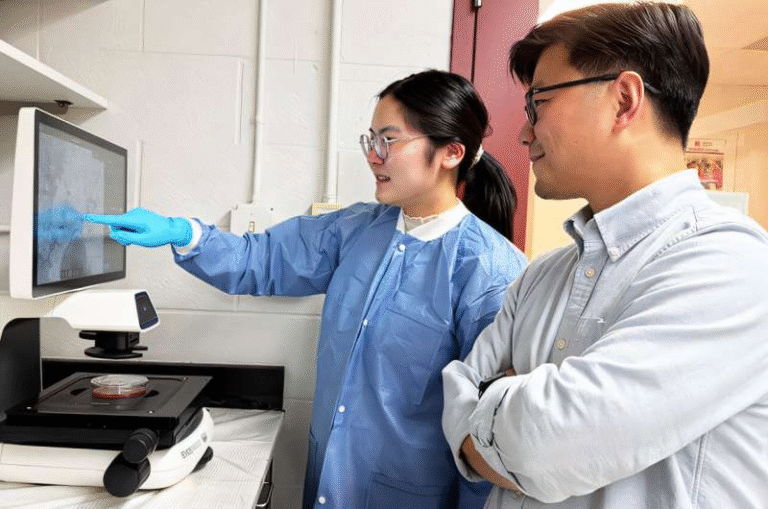
To investigate this idea, a research team led by scientists at Yale School of Medicine conducted a large-scale analysis combining symptom data and brain imaging. Their findings, published in the journal Biological Psychiatry, point to a more nuanced understanding of PTSD as a condition shaped by multiple emotional systems rather than a single fear-based response.
Two Distinct PTSD Symptom Profiles
The study identified two clear clinical profiles of PTSD, each with its own pattern of symptoms.
The first profile aligns closely with how PTSD is traditionally described. This fear-based profile includes symptoms linked to heightened threat detection and reactivity. Individuals in this group tend to experience flashbacks, intrusive memories, nightmares, exaggerated startle responses, distress when reminded of the trauma, and active avoidance of people, places, or situations associated with the traumatic event. These symptoms reflect an overactive fear system that remains stuck in survival mode long after the danger has passed.
The second profile looks quite different. The emotional pain profile is characterized by inward-facing distress rather than outward fear responses. People in this group often report a loss of interest in activities, persistent negative beliefs about themselves or the world, ongoing negative emotions such as guilt or shame, sleep disturbances, and heightened emotional sensitivity. These symptoms resemble deep psychological pain rather than immediate threat awareness.
One of the most striking findings from the study is how participants themselves rated the impact of these symptoms. Nearly 70 percent of those surveyed reported that emotional pain interfered with their daily lives more than fear-based symptoms. This suggests that emotional pain may be a major, and often overlooked, source of suffering in PTSD.
How the Study Was Conducted
The research involved two separate analyses using different participant groups and methods.
In the first analysis, more than 800 trauma-exposed individuals completed a standardized PTSD symptom checklist. Instead of simply measuring symptom severity, the researchers examined how different symptoms related to one another. This network-based approach revealed the two distinct symptom clusters—fear and emotional pain—emerging consistently across the data.
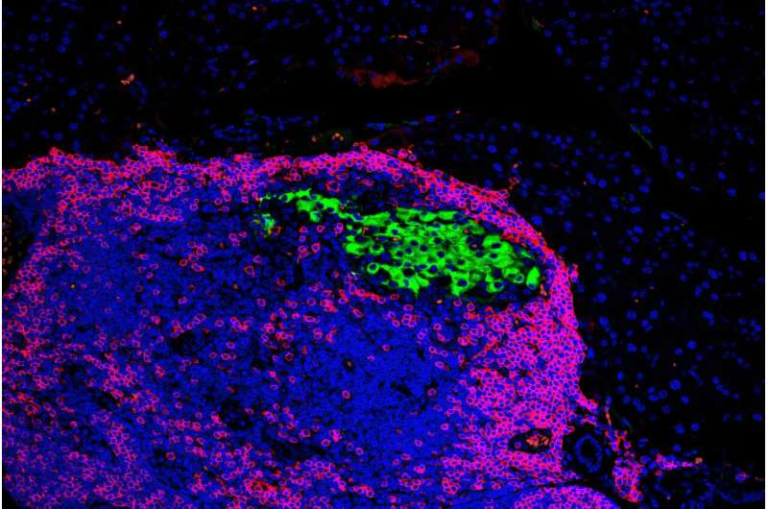
The second analysis focused on the brain. Using functional magnetic resonance imaging (fMRI), the researchers examined whole-brain connectivity patterns in 162 recent trauma survivors. Brain scans were conducted shortly after the traumatic event, and participants were followed over time. The goal was to see whether early brain connectivity patterns could predict symptom severity 14 months later.
Rather than concentrating on individual brain regions, the team analyzed large-scale brain networks and how they interact dynamically. This approach reflects a growing trend in neuroscience that emphasizes brain systems over isolated structures.
What the Brain Data Revealed
The brain imaging results added another layer of insight. The researchers found that early connectivity patterns in the brain were able to predict the severity of fear-based PTSD symptoms more than a year later. However, these same patterns did not predict emotional pain symptoms.
This difference is important. It suggests that fear and emotional pain in PTSD may be driven by different neural mechanisms. In other words, the brain circuits underlying fear-related symptoms may not be the same ones responsible for emotional pain.
Even though the imaging findings applied only to fear-based symptoms, the result actually strengthens the overall model. The fact that fear and emotional pain showed different neural signatures supports the idea that PTSD is not a single, uniform condition.
Importantly, these findings were consistent across two independent samples studied at different times and in different locations, increasing confidence that the fear-versus-emotional-pain distinction is robust and not a statistical fluke.
Why This Matters for PTSD Treatment
Current PTSD treatments—both medications and psychotherapies—are largely designed to reduce fear. Exposure therapy, for example, helps patients gradually confront trauma-related memories or situations in a safe environment to reduce fear responses. Many medications also target systems involved in anxiety and threat processing.
While these approaches can be effective for some individuals, they do not work for everyone. The new research offers a potential explanation for why. If a person’s PTSD is primarily driven by emotional pain rather than fear, treatments aimed solely at fear reduction may miss the core of their distress.
This insight supports a move toward precision psychiatry, an approach that tailors treatment to the specific emotional and biological profile of each individual. Instead of assuming that all PTSD patients need the same type of intervention, clinicians could focus on identifying whether fear or emotional pain is the dominant factor and adjust treatment strategies accordingly.
Emotional Pain and Mental Health More Broadly
Beyond PTSD, emotional pain is increasingly recognized as a central feature of many mental health conditions. Feelings such as shame, guilt, loss, and persistent negative self-beliefs are common across depression, anxiety disorders, and trauma-related conditions. These emotional states can be deeply disabling, even in the absence of overt fear or panic.
The Yale study adds to a growing body of research suggesting that mental health disorders may be better understood by examining core emotional processes rather than rigid diagnostic categories. By focusing on underlying emotional experiences, researchers and clinicians may be able to develop more targeted and effective treatments.
A Shift in How PTSD Is Viewed
This research does not dismiss the role of fear in PTSD. Fear remains a critical component for many individuals. What it does challenge is the idea that fear alone defines the disorder.
By recognizing emotional pain as a distinct and powerful driver of PTSD symptoms, the study encourages a broader, more inclusive understanding of trauma-related suffering. It also opens the door to new research directions, including identifying brain markers for emotional pain and developing therapies specifically designed to address it.
As PTSD research continues to evolve, this dual-profile model may help bridge the gap between neuroscience, clinical practice, and patient experience—bringing treatment closer to the realities of how people actually live with trauma.
Research paper: https://doi.org/10.1016/j.biopsych.2025.11.016