How Our Nasal Passages Defend Against the Common Cold and Influence How Sick We Get
When most of us think about the common cold, we usually picture sneezing, a runny nose, and a few miserable days of congestion. But behind those everyday symptoms, a surprisingly complex biological battle is happening inside our noses. New research shows that our nasal passages are not just passive entry points for viruses, but active defenders that play a major role in determining whether we get sick at all—and how severe our symptoms become.
Scientists studying rhinovirus, the most frequent cause of the common cold, have taken a close look at what happens when this virus infects the lining of the human nose. Their findings suggest something important: our body’s response to the virus often matters more than the virus itself.
Why Rhinovirus Matters So Much
Rhinoviruses are responsible for the majority of common cold cases worldwide. Beyond mild sniffles, they are also a major trigger for asthma attacks and breathing problems in people with chronic lung conditions. Despite being so common, rhinoviruses are tricky to study because they mainly infect humans and not other animals, limiting the usefulness of traditional animal models.
To overcome this, researchers turned their attention directly to the human nasal lining, where rhinovirus infections begin.
Building the Human Nose in the Lab
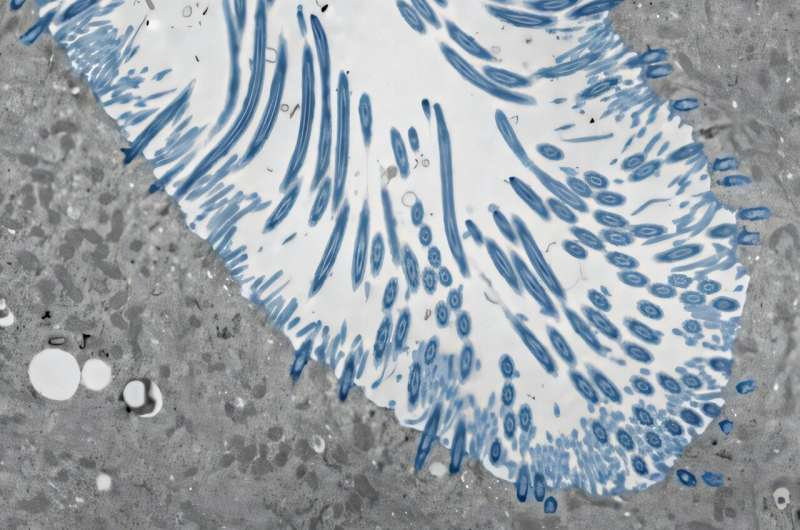
To study nasal defenses in detail, researchers created lab-grown human nasal tissue, known as organoids. These were developed from human nasal stem cells cultured over four weeks. During this time, the cells were exposed to air on their surface, allowing them to mature in a way that closely resembles real nasal tissue.
The resulting tissue contained many of the same cell types found in actual nasal passages and lung airways. These included mucus-producing cells, which trap viruses and debris, and ciliated cells, which use tiny hair-like structures to sweep mucus and trapped particles out of the airways.
This lab-grown tissue proved far more realistic than standard cell lines, making it possible to observe how thousands of individual cells respond together during a rhinovirus infection.
The Interferon Defense System
One of the most important discoveries from this research involves interferons, a group of proteins that act as powerful antiviral signals.
When nasal cells sense rhinovirus, they rapidly produce interferons. These interferons don’t just protect the infected cell—they also warn neighboring cells, triggering a coordinated antiviral defense across the tissue. This response makes the environment hostile to the virus, blocking its ability to enter cells and replicate.
If this interferon response happens quickly, the virus struggles to spread. In many cases, the infection is stopped before it causes noticeable symptoms. This helps explain why some people can be exposed to rhinovirus and barely feel sick, or not feel sick at all.
What Happens When Defenses Fail
The researchers also tested what happens when this interferon response is disrupted. When they experimentally blocked the cellular sensors responsible for detecting rhinovirus, the results were dramatic.
Without interferon signaling, the virus rapidly spread through the tissue, infecting many more cells. This led to significant tissue damage and, in some cases, the death of infected organoids. These experiments clearly showed that a fast and effective interferon response is critical for controlling rhinovirus infection—even in the absence of immune cells like white blood cells.
When Symptoms Get Worse
The study didn’t stop at interferons. Researchers also identified other defense pathways that activate when viral replication increases.
At higher levels of infection, rhinovirus can trigger a different sensing system in nasal cells. This system causes infected and uninfected cells to work together in ways that may actually worsen symptoms. These responses include excessive mucus production, increased inflammation, and airway irritation, all of which can contribute to congestion and breathing problems.
While these responses are still part of the body’s defense strategy, they may explain why some people experience severe cold symptoms, especially those with asthma or other respiratory conditions.
Why Some People Get Sicker Than Others
One of the most important takeaways from this research is that individual differences in immune response matter greatly. Two people exposed to the same rhinovirus strain may have very different outcomes—not because the virus behaves differently, but because their nasal tissues respond differently.
A rapid, well-controlled interferon response can limit infection and reduce symptoms. A slower or weaker response allows the virus to spread, triggering stronger inflammatory reactions that lead to more noticeable illness.
This shifts the focus away from the virus alone and toward the host’s biology as a key factor in cold severity.
A Closer Look at the Nasal Lining
The nasal lining is more than just a physical barrier. It is an active immune organ equipped with sensors that detect invading pathogens almost instantly. These sensors initiate signaling pathways that balance antiviral protection with inflammation.
In everyday life, this balance is crucial. Too little response allows the virus to spread, while too much inflammation can cause discomfort and breathing issues. Understanding how this balance is regulated opens the door to new strategies for managing respiratory infections.
Implications for Future Treatments
Rather than trying to eliminate rhinovirus directly—a difficult task given the many strains—this research points to another promising approach: supporting and fine-tuning the body’s natural defenses.
Therapies that enhance early interferon responses or limit harmful inflammation could potentially reduce symptoms and prevent complications, especially in people with asthma or chronic lung disease. Targeting these defense mechanisms may be more effective than traditional antiviral strategies.
Limitations and What Comes Next
While the lab-grown nasal organoids closely mimic real tissue, they still have limitations. They contain fewer cell types than a living human nose and lack immune cells that would normally be recruited during infection.
Future studies aim to explore how immune cells, environmental factors, and repeated viral exposure influence nasal defenses. This will help researchers better understand how real-world infections unfold and how the body calibrates its response over time.
Expanding Our Understanding of the Common Cold
This research reinforces a growing idea in medicine: illness severity is often shaped by the body’s response, not just the pathogen. In the case of the common cold, our noses are doing far more than we once realized—quietly coordinating defenses that determine whether we shrug off a virus or spend days reaching for tissues.
By focusing on the nasal passages, scientists are uncovering new insights that could change how we think about, prevent, and treat one of the most familiar illnesses in human life.
Research Paper:
https://www.sciencedirect.com/science/article/pii/S3051383925000015





