A Protein in the GI Tract Can Neutralize Many Bacteria and Strengthen the Body’s Natural Defenses
The human body is constantly interacting with trillions of microbes, especially along the mucosal surfaces that line organs such as the gut, lungs, and nasal passages. These surfaces are not passive barriers. They are active, dynamic systems packed with molecules that help manage microbes and prevent unnecessary inflammation or infection. New research from scientists at MIT highlights one such molecule—a protein in the gastrointestinal tract that can both reinforce the gut’s mucus barrier and directly neutralize harmful bacteria.
The protein is called intelectin-2, and according to this study, it has a surprisingly broad role in protecting the gut. Researchers found that it doesn’t just sit back and wait for bacteria to cause trouble. Instead, it works in two complementary ways, strengthening the body’s first line of defense and stepping in directly when that defense is compromised.
The Role of Mucosal Surfaces in Immune Defense
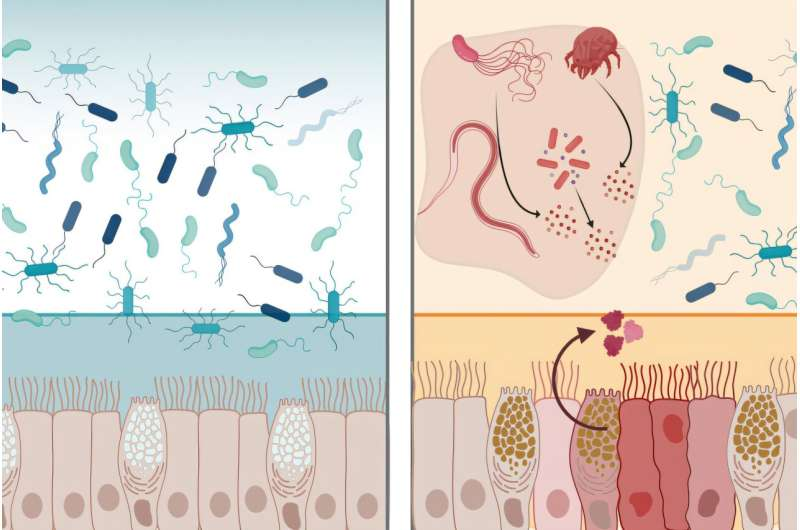
Mucosal surfaces are among the most vulnerable parts of the body. The gastrointestinal tract, in particular, is exposed daily to foodborne microbes, pathogens, and trillions of resident bacteria. To manage this, the gut relies heavily on mucus, a gel-like layer made primarily of molecules called mucins.
This mucus layer acts as a physical and chemical shield, keeping microbes at a safe distance from the intestinal lining. Embedded within this mucus are many defensive molecules, including lectins—proteins that recognize and bind to specific sugar structures found on cells and microbes.
Lectins are known for their ability to identify “self” versus “non-self”, making them valuable players in immune defense. The human genome encodes more than 200 different lectins, each with specialized roles ranging from immune signaling to microbial recognition.
What Makes Intelectin-2 Special
Intelectin-2 belongs to a small family of lectins called intelectins. Humans produce two versions: intelectin-1 and intelectin-2. While the two proteins have very similar structures, they behave differently.
Intelectin-1 is known to bind only to carbohydrates found on bacteria and other microbes, but its exact role in immune defense is still not fully understood. Intelectin-2, on the other hand, has been less studied—until now.
In this research, scientists closely examined intelectin-2 and discovered that it has broad-spectrum antimicrobial activity against many bacteria found in the GI tract. What stood out was not just its ability to interact with bacteria, but the versatility of how it works.
Strengthening the Mucus Barrier
One of the most important findings is that intelectin-2 binds to a sugar called galactose. Galactose is commonly found on mucins, the molecules that give mucus its structure.
When intelectin-2 binds to these galactose-containing mucins, it can crosslink them, effectively reinforcing and stabilizing the mucus layer. This makes the barrier tougher and more resistant to disruption.
In healthy tissue, this function appears to be the protein’s primary role—maintaining the integrity of the mucus layer so bacteria remain trapped at a safe distance from intestinal cells.
Directly Neutralizing Bacteria When the Barrier Fails
The second function of intelectin-2 becomes critical when the mucus barrier is weakened, such as during inflammation or infection. Galactose is not exclusive to mucus. Many bacteria also display galactose-containing carbohydrates on their cell surfaces.
The researchers showed that intelectin-2 can bind directly to these bacteria, trapping them within the mucus and preventing them from spreading or multiplying. Over time, the trapped microbes begin to disintegrate, suggesting that the protein disrupts their cell membranes.
This antimicrobial activity affects a wide range of bacteria, including several known to cause gastrointestinal infections. Importantly, some of these bacteria are resistant to traditional antibiotics, making intelectin-2 especially interesting from a medical perspective.
Expression in Humans and Mice
The study also explored where and when intelectin-2 is produced. In humans, the protein is made at steady levels by Paneth cells in the small intestine. These cells are already known for producing antimicrobial compounds, so intelectin-2 fits well into their defensive toolkit.
In mice, the situation is slightly different. There, intelectin-2 is produced by goblet cells, which are responsible for mucus secretion. Its expression increases during inflammation and certain parasitic infections, suggesting that the protein is part of a responsive defense system that ramps up when the gut is under threat.
Why This Matters for Gut Disorders
The findings have important implications for conditions such as inflammatory bowel disease (IBD). In people with IBD, intelectin-2 levels can become abnormally high or low.
Low levels may weaken the mucus barrier, allowing bacteria to come into direct contact with intestinal cells and trigger inflammation. High levels, on the other hand, could be harmful by killing too many beneficial gut bacteria, disrupting the delicate balance of the gut microbiome.
This highlights how critical it is to maintain the right amount of intelectin-2. Therapies that restore or fine-tune its levels could help stabilize the mucus barrier and reduce inflammation in patients with chronic gut disorders.
A New Direction for Antimicrobial Strategies
Beyond gut health, intelectin-2 opens the door to new antimicrobial approaches. Because it is a protein the human body already produces, it represents a strategy that works with the immune system, not against it.
Unlike antibiotics, which target specific bacterial processes and often drive resistance, lectins like intelectin-2 act by binding to surface sugars—structures that are harder for bacteria to alter without compromising their survival.
Researchers believe this makes intelectin-2 a promising candidate for developing novel antimicrobial therapies, especially against pathogens such as Staphylococcus aureus and Klebsiella pneumoniae, which are notoriously difficult to treat.
The Bigger Picture of Lectins in Immunity
This study also reinforces the broader importance of lectins in human health. Far from being simple sugar-binding proteins, lectins are emerging as multifunctional immune tools that help shape microbial communities, reinforce physical barriers, and directly combat pathogens.
Understanding how lectins like intelectin-2 work could lead to engineered proteins or treatments that mimic their natural functions, offering new ways to protect mucosal surfaces without disrupting beneficial microbes.
Looking Ahead
Intelectin-2 shows how the body’s own defenses are often more sophisticated than we realize. By stabilizing the mucus barrier and neutralizing bacteria when needed, this single protein plays a dual role that is both elegant and effective.
As antibiotic resistance continues to rise, discoveries like this point toward a future where therapies are inspired by innate immune mechanisms, using strategies the body has refined over millions of years.
Research Paper:
https://www.nature.com/articles/s41467-025-67099-4