Vitamin B3 Shows Promise in Reversing Fatty Liver Disease

A major new study has revealed that vitamin B3 (niacin) could play a critical role in tackling one of the most widespread liver conditions in the world — metabolic dysfunction-associated steatotic liver disease (MASLD), previously known as non-alcoholic fatty liver disease (NAFLD). The research team, involving scientists from UNIST (Ulsan National Institute of Science and Technology), Pusan National University, and Ulsan University Hospital, has identified a specific genetic factor driving this disease and shown how niacin can suppress its harmful effects.
Let’s break down all the details of this discovery, what makes it important, and why it could reshape how MASLD is treated.
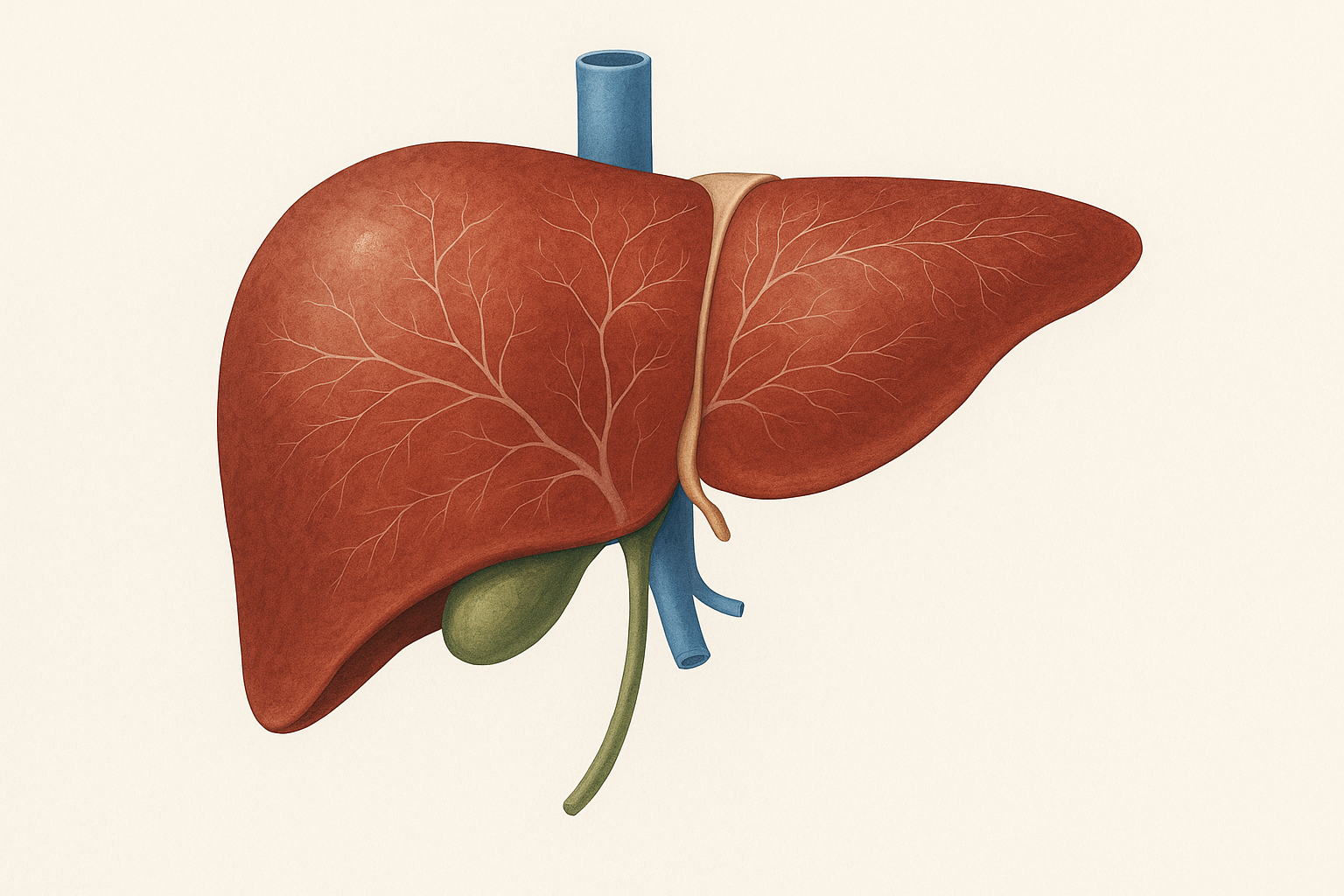
What is MASLD?
MASLD, short for metabolic dysfunction-associated steatotic liver disease, is a condition where excess fat builds up in the liver in people who do not drink alcohol heavily. It is estimated that around 30% of the global population is affected, making it the most common chronic liver condition in the world.
The disease develops largely due to obesity, insulin resistance, sedentary lifestyle, and poor diet. Over time, MASLD can progress to more severe forms such as metabolic dysfunction-associated steatohepatitis (MASH), which involves inflammation and liver cell damage. Eventually, some patients may experience fibrosis, cirrhosis, and even liver cancer.
The worrying part is that MASLD has no highly effective targeted therapy yet. Treatment mainly revolves around lifestyle changes, such as weight loss and increased physical activity. Some drugs are being studied, but none have become widely established as first-line therapies.
That is why new research into the molecular triggers of the disease — and potential ways to block them — is so crucial.
The Discovery: miR-93 as a Genetic Driver
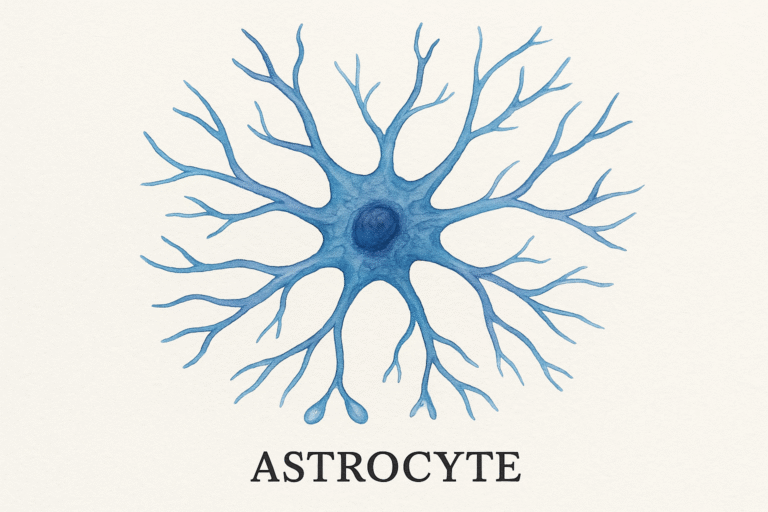
The new study zeroed in on a molecule called microRNA-93 (miR-93). MicroRNAs are short pieces of RNA that regulate how genes are expressed, effectively acting as switches that can turn certain processes on or off.
In this case, researchers discovered that miR-93 levels are unusually high in the livers of both human MASLD patients and animal models of the disease. This elevation turns out to be bad news for liver health.
What miR-93 does in the liver
- Suppresses SIRT1: miR-93 directly blocks a gene known as SIRT1, which is essential for maintaining healthy lipid metabolism.
- Disrupts lipid balance: With SIRT1 suppressed, fat begins to accumulate inside liver cells, causing steatosis.
- Triggers inflammation and fibrosis: Over time, the imbalance also worsens inflammation and fibrosis, accelerating the progression of MASLD.
The study showed that when scientists genetically deleted miR-93 in mice using CRISPR/Cas9 gene-editing, the mice were protected from developing fatty liver, even when fed high-fat, high-fructose diets.
These knockout mice not only had less fat in the liver but also displayed:
- Better glucose tolerance
- Improved insulin sensitivity
- Healthier mitochondrial function
- Reduced markers of liver injury
On the other hand, when mice were engineered to overproduce miR-93 in the liver, the exact opposite happened. Their liver fat content increased, glucose and insulin metabolism worsened, and signs of liver damage went up significantly.
This confirmed miR-93 as a key driver of fatty liver disease.
Vitamin B3 as the Game-Changer
After establishing the harmful role of miR-93, the researchers turned to the question: Can this molecule be suppressed safely?
They screened 150 FDA-approved drugs to see which compound could best suppress miR-93 in the liver. The clear winner was niacin (vitamin B3).
Why niacin works
- Suppresses miR-93: Niacin treatment lowered hepatic levels of miR-93 in animal models.
- Boosts SIRT1 activity: With less miR-93 interference, SIRT1 was reactivated.
- Restores lipid balance: Liver cells regained their ability to regulate fat metabolism properly.
- Improves metabolic health: Mice treated with niacin showed reduced steatosis, better insulin sensitivity, improved glucose handling, and overall improved liver function.
This is especially significant because niacin is already widely used as a treatment for hyperlipidemia (high cholesterol and triglycerides). It has a long history of medical use, and its safety profile is well-established at therapeutic doses.
The findings suggest that niacin could be repurposed as a therapy for MASLD, either as a standalone treatment or in combination with other drugs.
The Mechanism: SIRT1 and AMPK Pathways
To understand how niacin works here, it helps to look at the role of SIRT1.
SIRT1 is a gene that influences multiple pathways related to energy metabolism. One key pathway it regulates is the LKB1-AMPK signaling pathway, which helps the liver burn fat efficiently and reduces fat storage.
When miR-93 suppresses SIRT1, this pathway is blocked, leading to lipid buildup and poor mitochondrial function.
Niacin’s effect on lowering miR-93 effectively removes this blockade, allowing SIRT1 to activate AMPK again. This restores fatty acid oxidation, reduces cholesterol synthesis, and improves overall energy balance in the liver.
The Bigger Picture: Why This Matters
There are several reasons why this research is so significant:
- First targeted approach: Most MASLD treatments are lifestyle-based. This is one of the first studies to identify a specific genetic target (miR-93) that drives the disease and show how it can be suppressed.
- Repurposing a known drug: Since niacin is already FDA-approved, the pathway to clinical use may be faster and cheaper than developing a completely new drug.
- Translational potential: The findings in mice are strong and mechanistically clear. While human trials are still needed, the translational potential is high.
- Broad implications for miRNA therapy: This research highlights the importance of microRNAs in liver disease. Therapies aimed at miRNAs (either blocking or enhancing them) could open new doors in treating not only MASLD but also other metabolic and inflammatory diseases.
What About Niacin in Humans?
Niacin has already been studied in humans for its cardiovascular benefits. At high doses, it can lower triglycerides, raise HDL (good cholesterol), and reduce LDL (bad cholesterol).
Some observational studies have hinted at benefits in fatty liver patients:
- Higher dietary niacin intake in MASLD patients has been linked with lower all-cause mortality, although the link with cardiovascular mortality is less clear.
- Animal studies have shown that niacin can reduce fat accumulation and inflammation in the liver.
However, there are caveats:
- Side effects: Niacin can cause flushing, gastrointestinal discomfort, and at very high doses, liver toxicity.
- Dose concerns: The doses needed to suppress miR-93 effectively in humans are not yet clear.
- Disease stage: It remains to be seen whether niacin is most useful in early MASLD, or whether it could also help patients with advanced fibrosis or cirrhosis.
MASLD in Context
To give readers a fuller understanding, let’s zoom out briefly on MASLD.
- Global prevalence: Affects nearly a third of adults worldwide. Rates are rising rapidly in parallel with obesity and type 2 diabetes.
- Risk factors: Obesity, insulin resistance, high-fat diets, excessive fructose intake, and sedentary lifestyle are the biggest drivers.
- Progression: Not all patients with MASLD will progress to MASH or cirrhosis, but those who do face serious complications, including liver cancer and the need for transplantation.
- Current treatments: Weight loss (5–10% of body weight) is the most effective intervention known so far. Some drugs, like GLP-1 agonists (used in diabetes), are showing promise in trials, but none are yet officially approved for MASLD.
Where Do We Go From Here?
The next steps will involve clinical trials to test niacin’s ability to suppress miR-93 in humans and measure its impact on MASLD patients. Researchers will need to carefully assess safety, dosing, and whether niacin can actually reverse or halt fibrosis in human livers.
Other miRNA-targeted approaches may also emerge. For example, antisense oligonucleotides designed to block specific miRNAs could offer highly precise treatments in the future.
For now, though, this study provides a clear proof of concept: a simple, well-known vitamin could be repurposed to fight one of the world’s most common liver diseases.
Final Thoughts
This discovery is exciting because it blends genetic insight with a practical therapeutic option. Identifying miR-93 as a harmful regulator in fatty liver disease gives researchers a clear target, and showing that niacin can counteract it provides a direct path to treatment possibilities.
As the prevalence of MASLD continues to climb worldwide, breakthroughs like this are urgently needed. While much more research is required before niacin can be prescribed as a liver treatment, the study represents a significant step forward in understanding and potentially managing fatty liver disease.