Heart Attacks May Be Linked to Hidden Infections: New Research Opens Surprising Possibilities

Heart disease has always been thought of as a lifestyle and genetics-driven condition, but new research suggests there may be more to the story. Scientists from Finland and the UK have uncovered compelling evidence that bacteria hiding in our arteries could play a key role in triggering heart attacks. This study, published in the Journal of the American Heart Association on August 6, 2025, points to the possibility that heart attacks may, in some ways, be infectious events. Even more fascinating, researchers believe that one day, vaccines could help prevent them.
This finding does not replace the conventional understanding of coronary artery disease—where cholesterol buildup, high blood pressure, smoking, and diabetes are central players—but it adds a new infectious twist that could reshape prevention and treatment. Let’s break down what the researchers found, how they reached their conclusions, and what it could mean for the future of cardiovascular medicine.
The Core Discovery: Bacteria in Arterial Plaques
The study examined tissue samples from two groups:
- 121 individuals who had died suddenly from cardiac causes.
- 96 surgical patients with atherosclerosis undergoing endarterectomy procedures to clear blocked arteries.
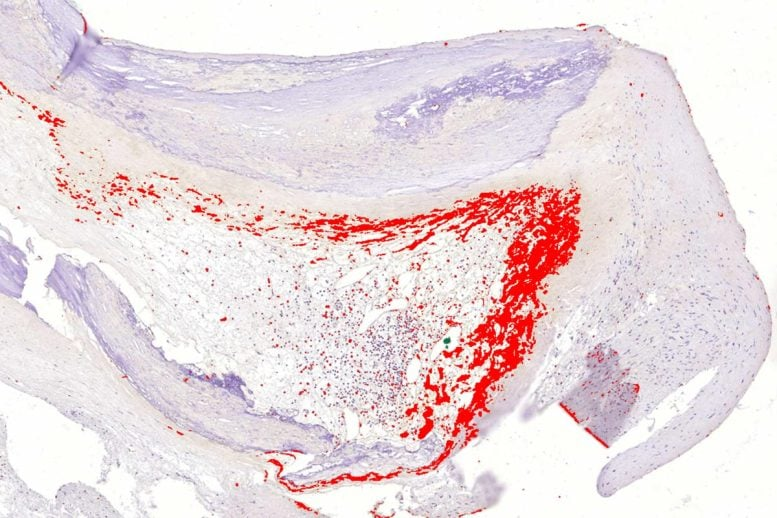
Using advanced tools like real-time quantitative PCR (RT-qPCR) and immunohistochemistry, researchers identified bacterial DNA deep inside cholesterol-rich plaques. They found that viridans group streptococci—a type of bacteria commonly found in the mouth—were present in a striking percentage of samples.
To be precise:
- Around 65% of coronary plaques from sudden-death cases contained bacterial DNA.
- About 58% of surgical specimens tested positive as well.
- Viridans streptococci DNA appeared in 42–43% of plaques overall.
- Immunohistochemistry confirmed bacterial presence in 60% of sudden-death plaques and 53% of surgical plaques.
This is not the first time scientists have suspected microbes in heart disease, but previous evidence was inconsistent. What makes this study different is the clear demonstration of bacterial DNA and biofilm structures right inside arterial tissue.
Biofilms: The Bacteria’s Hidden Stronghold
The bacteria weren’t floating freely. Instead, they formed biofilms—dense jelly-like communities that allow microbes to live together in a protective matrix. These biofilms:
- Hide bacteria from the immune system.
- Block antibiotic penetration, making them nearly impossible to kill with standard drugs.
- Can persist silently for decades, causing no symptoms while the plaque grows.
Researchers noticed that these biofilms were deep in the core of atherosclerotic plaques, shielded from the body’s normal defenses. This positioning allowed bacteria to remain undetected while the plaque gradually became unstable.
What Triggers the Bacteria?
One of the most intriguing findings is the idea of a “wake-up call.” The bacteria in the biofilm may stay dormant for years until triggered. According to the researchers, viral infections or other external stresses can activate these biofilms.
When the biofilm disperses, bacteria are suddenly exposed to the immune system. This sparks inflammation, a process that weakens the thin fibrous cap covering the plaque. If the cap ruptures, the underlying cholesterol and tissue contents spill into the bloodstream, forming a clot that blocks blood flow—and that’s the recipe for a heart attack.
This mechanism helps explain why some people suffer heart attacks shortly after viral illnesses such as the flu. Instead of being a coincidence, the infection could be the exact event that disturbs long-dormant bacteria.
The Role of the Immune System
The team also looked at how the immune system responds when bacteria are released from their protective biofilm. They found that:
- Toll-like receptors (TLRs), especially TLR2, recognize the bacterial components.
- This sets off innate immune responses, the body’s first line of defense.
- In advanced plaques, signs of both innate and adaptive immune activation were visible near rupture sites.
Importantly, immunopositivity (evidence of bacterial presence in tissue) strongly correlated with more severe plaque damage, fatal coronary heart disease, and myocardial infarction.
Why This Study Matters
This research suggests that bacteria might be active participants in plaque destabilization, not just passive bystanders. That changes how we think about heart disease in several ways:
- New Diagnostics – If bacterial biofilms mark vulnerable plaques, we may one day have blood tests or imaging tools that identify high-risk patients more accurately than cholesterol tests alone.
- New Therapies – Instead of only lowering cholesterol, future treatments could target biofilms or bacteria directly. This might involve antibiofilm drugs, immune-modulating therapies, or even tailored antimicrobials.
- Vaccination Potential – Since the bacteria identified are common oral microbes, vaccines could theoretically reduce their ability to colonize arteries. Preventing infection might prevent heart disease decades later.
Study Background and Support
This large-scale project involved collaboration between Tampere University, Oulu University, the Finnish Institute for Health and Welfare, and the University of Oxford. The study was also part of an EU-funded cardiovascular project involving 11 countries, with additional funding from the Finnish Foundation for Cardiovascular Research and the Jane and Aatos Erkko Foundation.
Such broad collaboration underscores the significance of the findings. Cardiovascular disease remains the leading cause of death worldwide, so any insight into previously overlooked contributors is of enormous public health interest.
Adding Perspective: The Bigger Picture
Heart Disease Basics
Heart attacks, medically called myocardial infarctions, occur when blood flow to part of the heart muscle is blocked, usually by a clot. Risk factors include:
- High levels of low-density lipoprotein (LDL) cholesterol
- Smoking
- High blood pressure
- Diabetes
- Obesity
- Family history
- Lack of physical activity
Until now, bacteria were not considered major players in this process. This study challenges that idea.
Oral Health and Heart Disease
Interestingly, oral health has long been linked to heart disease. People with gum disease (periodontitis) are at higher risk of cardiovascular problems. One theory is that oral bacteria enter the bloodstream during everyday activities like brushing or chewing, especially when gums are inflamed.
The fact that viridans streptococci, common in the mouth, were identified in arterial plaques strengthens this link. This could mean good oral hygiene is more important for heart health than we ever realized.
The Challenge of Biofilms
If bacteria in heart plaques live in biofilms, that presents a major therapeutic challenge. Biofilms are notoriously difficult to destroy because:
- The protective matrix blocks drugs.
- Bacteria inside grow slowly, making them less susceptible to antibiotics.
- Standard immune defenses cannot penetrate.
New strategies may be required, such as enzymes that break down biofilms, novel antimicrobial peptides, or approaches that disrupt bacterial communication systems known as quorum sensing.
Vaccination: A Future Possibility
The most exciting long-term implication is vaccination. Imagine a world where, alongside vaccines for measles or influenza, people receive a vaccine to protect against bacteria linked to heart disease. If successful, this could revolutionize prevention.
That said, developing such a vaccine would not be simple. Viridans streptococci are also part of the normal oral microbiome. Completely wiping them out might have unintended effects. Any vaccine would need to be carefully targeted to avoid disturbing beneficial bacteria.
Important Caveats
Before getting carried away, it’s important to highlight the limits of this research:
- Correlation vs. causation: Just because bacteria are present in plaques doesn’t prove they caused the rupture. They may have colonized already damaged tissue.
- Speculative triggers: The link between viral infections and biofilm activation is plausible but not definitively proven.
- Treatment challenges: Biofilms are very resistant to treatment, and reaching them inside plaques adds another layer of difficulty.
- Conventional risk factors still matter: High cholesterol, hypertension, smoking, and other lifestyle factors remain well-established drivers of heart disease.
In short, this study opens an exciting new direction, but it doesn’t replace what we already know.
Conclusion
This research sheds light on a fascinating and unexpected contributor to heart attacks: bacterial biofilms hiding in arterial plaques. By evading detection for years and then triggering inflammation at critical moments, these microbes may help explain why heart attacks often occur suddenly—even in people who seemed relatively stable.
If confirmed by further studies, the implications are enormous. We might one day diagnose vulnerable plaques more accurately, develop antibiofilm therapies, and even vaccinate people against heart attacks.
For now, the best advice remains the same: maintain good oral hygiene, control cholesterol, exercise, eat healthily, and avoid smoking. But keep an eye on this research—it could reshape our entire understanding of cardiovascular disease.