Very Few Americans Use Salt Substitutes Despite Clear Benefits for Blood Pressure

A major new analysis presented at the American Heart Association’s Hypertension Scientific Sessions 2025 has highlighted a surprisingly underused tool in the fight against high blood pressure: salt substitutes.
Even though these alternatives to regular salt are inexpensive, easy to use, and shown to help reduce sodium intake, fewer than 6% of U.S. adults report using them. This finding is based on nearly two decades of data from the National Health and Nutrition Examination Survey (NHANES), covering the years 2003 through early 2020.
Let’s break down exactly what this study found, why it matters, and what it means for public health moving forward.
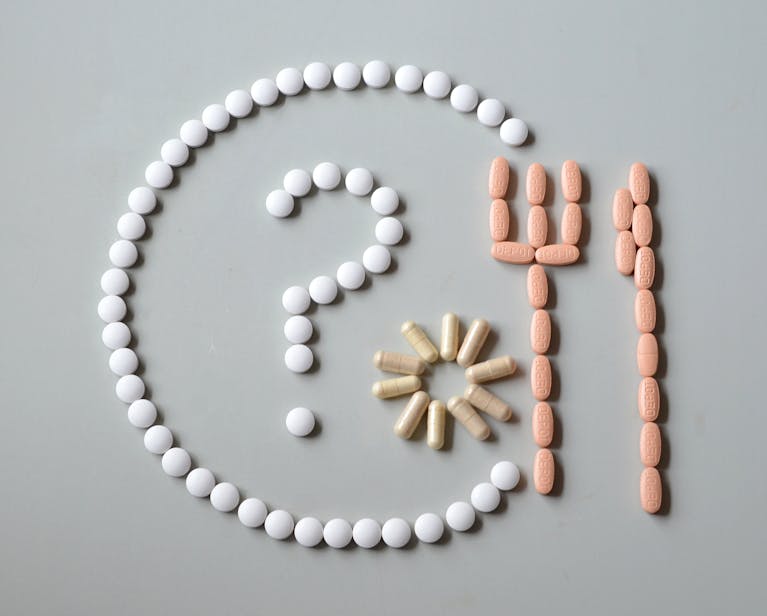
What Are Salt Substitutes?
Salt substitutes are products in which some or all of the sodium chloride (NaCl) is replaced with potassium chloride (KCl) or other mineral salts. The taste is often very similar to regular table salt, though potassium-based substitutes can sometimes leave a slight bitter aftertaste when heated.
Most sodium in the average American diet doesn’t come from a salt shaker at the table but from processed and packaged foods and restaurant meals. Salt substitutes can reduce sodium consumption while also increasing potassium intake, a combination known to support heart health and lower blood pressure.

The American Heart Association (AHA) recommends limiting sodium to no more than 2,300 mg per day, with an ideal goal of under 1,500 mg per day, especially for people with high blood pressure. Even reducing daily sodium intake by 1,000 mg can lead to measurable improvements in blood pressure and cardiovascular risk.
The Scope of High Blood Pressure in the U.S.
High blood pressure, or hypertension, is one of the most common chronic health conditions in the United States. According to survey data between 2017 and 2020, an estimated 122.4 million adults—that’s 46.7% of the adult population—were living with hypertension. During that same period, it contributed to more than 130,000 deaths.
Hypertension develops when the force of blood pushing against artery walls stays consistently elevated. Over time, this places enormous strain on the heart, blood vessels, kidneys, and brain. It is a leading risk factor for heart attacks, strokes, kidney disease, and heart failure. Both excess sodium and insufficient potassium intake are well-established dietary contributors.
What the Study Looked At
The research team, led by Yinying Robyn Wei, M.C.N., R.D.N., L.D., and Ph.D. candidate at UT Southwestern Medical Center in Dallas, wanted to know how many Americans actually use salt substitutes, and whether usage has changed over time.
The analysis included 37,080 adults aged 18 and older, broken down as follows:
- 37.9% were ages 18–39
- 36.9% were ages 40–59
- 25.2% were ages 60 and older
- 50.6% were women
- 10.7% self-reported as non-Hispanic Black
- 89.3% self-reported as other racial and ethnic groups
Participants were categorized into four subgroups based on their blood pressure and whether they were taking blood pressure medications:
- High blood pressure, treated and controlled
- High blood pressure, treated but not controlled
- Untreated high blood pressure
- Normal blood pressure
The researchers considered three categories of salt use:
- Ordinary salt (table salt, sea salt, kosher salt, iodized salt)
- Salt substitutes (potassium-enriched or other alternatives)
- No salt use
They also ran a secondary analysis focusing only on people considered eligible for salt substitutes: those with normal kidney function (estimated glomerular filtration rate ≥ 60) and not taking medications or supplements that affect potassium levels. This is important because some salt substitutes can be risky for people with kidney disease or those on medications that increase potassium, since too much potassium can lead to dangerous heart rhythm problems.
The Findings in Detail
Here’s what the researchers found after reviewing nearly two decades of survey responses:
- Overall use is low: Salt substitute use across all U.S. adults remained consistently low. It peaked at 5.4% in 2013–2014 but dropped to just 2.5% by 2017–March 2020. Data collection for 2020 ended early due to the pandemic.
- Eligible adults still barely use them: Among those who were medically safe to use salt substitutes, only 2.3% to 5.1% reported doing so.
- Highest use among controlled hypertension patients: People with high blood pressure that was treated and controlled with medication reported the highest use—between 3.6% and 10.5%.
- Uncontrolled hypertension still low usage: Among those whose high blood pressure remained uncontrolled despite medication, usage was between 3.7% and 7.4%.
- Untreated and normal BP groups: Both groups consistently showed salt substitute usage of less than 5.6%.
- Restaurant habits don’t predict much: Adults who ate at restaurants three or more times a week were less likely to use salt substitutes, but once adjustments were made for factors like age, race, education, and insurance, the difference was no longer statistically significant.
Overall, the message is clear: salt substitute use is rare in the U.S., even among people who stand to benefit the most.
Why Aren’t More People Using Them?
The study did not directly measure why people avoid or overlook salt substitutes, but it raises several possibilities:
- Taste acceptance: Some people notice a difference in flavor, especially when cooking with heat, since potassium-based salts can develop a bitter aftertaste.
- Cost and availability: Although inexpensive compared to other health interventions, salt substitutes may not be widely available in all grocery stores.
- Lack of awareness: Many patients (and even some clinicians) may not know salt substitutes exist or how they can be used safely.
- Safety concerns: Since not everyone can use them—particularly those with kidney issues or on certain medications—there may be hesitation.
The researchers emphasized that healthcare professionals could play a major role by discussing salt substitutes during visits, particularly for patients with difficult-to-control hypertension.
Limitations of the Study
Like all research, this study has some caveats:
- Self-reported data: Participants reported their own salt substitute use, which could lead to underreporting or misclassification.
- Lumped categories: All salt substitutes were grouped together, so the researchers couldn’t separate potassium-enriched salts from other non-sodium salts.
- No dosage information: The survey did not capture how much salt substitute people were actually using, so the true impact on sodium and potassium intake remains unclear.
Despite these limitations, the data provide valuable insight into long-term trends and raise important questions for public health efforts.
Why This Matters
High blood pressure is often called the “silent killer” because it rarely causes noticeable symptoms until serious complications arise. Controlling it requires a combination of medication, lifestyle changes, and dietary adjustments. One of the simplest dietary changes—using a salt substitute instead of regular salt—remains severely underused.
This is an opportunity gap. Increasing awareness, ensuring availability, and educating both patients and healthcare providers could make a meaningful difference in public health. Even a modest shift away from sodium chloride toward potassium chloride could help reduce the burden of heart disease and stroke in the U.S.
Extra Knowledge: Sodium, Potassium, and Blood Pressure
To better understand why salt substitutes matter, it helps to know how sodium and potassium work in the body:
- Sodium: Excess sodium causes the body to retain water, which increases blood volume and raises blood pressure.
- Potassium: Potassium helps relax blood vessel walls and allows the body to excrete sodium through urine, counterbalancing sodium’s harmful effects.
This sodium–potassium balance is crucial. Unfortunately, most Americans consume too much sodium (over 3,400 mg per day on average) and too little potassium (less than the recommended 4,700 mg per day). Salt substitutes help tip this balance in the right direction.
What You Can Do
If you have normal kidney function and are not on medications that affect potassium levels, consider trying a salt substitute. But always check with your healthcare provider first, especially if you have health conditions or are on medications that could affect potassium levels.
For those who cannot use potassium-based salt substitutes, other strategies include:
- Reducing processed and packaged food intake
- Cooking at home more often
- Using herbs, spices, lemon juice, and vinegar to flavor food instead of relying on salt
Looking Ahead
The researchers recommend further studies to explore barriers to adoption. Is it mainly a matter of taste, cost, or lack of awareness? Understanding these factors could guide public health campaigns and clinical strategies to promote salt substitutes where safe and appropriate.
At the population level, even a small increase in adoption could lead to significant improvements in blood pressure control and reductions in heart disease, stroke, and premature death.
Conclusion
The bottom line: less than 6% of U.S. adults use salt substitutes, despite clear evidence of their benefits for blood pressure and heart health. Usage has remained stagnant or even declined over the last two decades. This represents a missed opportunity in addressing the widespread problem of hypertension.
With nearly half of American adults living with high blood pressure, the stakes are high. Encouraging wider, safer use of salt substitutes could be a simple but powerful step in improving cardiovascular health nationwide.
Research Source: American Heart Association – Hypertension Scientific Sessions 2025: U.S. survey finds salt substitutes rarely used by people with high blood pressure