World’s First Perovskite Camera Could Transform Nuclear Medicine Imaging

A major breakthrough has just been announced in the field of nuclear medicine imaging: scientists from Northwestern University in the United States and Soochow University in China have developed the world’s first perovskite-based gamma-ray detector, often described as a perovskite camera. This new technology promises to make medical scans like SPECT (Single-Photon Emission Computed Tomography) faster, clearer, safer, and significantly more affordable.
This detector is not just a small improvement—it could change how doctors around the world use nuclear imaging to diagnose diseases. It combines better resolution, higher sensitivity, lower radiation doses, and reduced costs, all in one package. Let’s break down the details of what this technology is, why it matters, how it was achieved, and what it could mean for the future.
Why Nuclear Medicine Matters
Nuclear medicine is one of the most powerful diagnostic tools available today. Unlike traditional X-rays or CT scans that only show structures, nuclear medicine can visualize biological activity inside the body.
For example:
- Doctors can watch how the heart pumps.
- They can follow blood flow patterns in real time.
- They can detect diseases hidden deep inside tissues, often long before structural damage is visible.
The most common techniques are SPECT and PET scans, both of which rely on introducing a small amount of a radiotracer into the patient’s body. This radiotracer emits gamma rays, which pass through tissue and are then captured by detectors outside the body. Each gamma ray is like a tiny pixel of light. By capturing millions of them, a computer reconstructs a 3D image of organ function.
But there’s a big limitation: the detectors themselves.
Current Detectors and Their Problems
Today’s nuclear medicine imaging relies mostly on two types of detectors:
- Cadmium Zinc Telluride (CZT):
- Extremely precise and capable of direct gamma-ray detection.
- Very expensive, often costing hundreds of thousands to millions of dollars per camera.
- Brittle and difficult to manufacture.
- Sodium Iodide (NaI) coupled with photomultipliers:
- Cheaper and more widely available.
- Bulkier and less precise, often producing blurry images, much like looking through a foggy window.
Because of these drawbacks, high-quality nuclear imaging is often limited to hospitals that can afford the best equipment. Many clinics rely on older, less precise systems, which means patients don’t always get the clearest or fastest scans.
The Role of Perovskites
This is where perovskites come into the picture. Perovskites are a family of crystals that have been studied intensively over the past decade, mostly because they revolutionized solar energy research.
- In 2012, Northwestern researchers made the first solid-film solar cells using perovskites.
- By 2013, they showed that single perovskite crystals could detect X-rays and gamma rays.
- Since then, the material has been recognized as a highly adaptable semiconductor with impressive electronic and optical properties.
What makes perovskites appealing is that they are easier to grow, simpler to process, and less expensive compared to CZT crystals, while still offering excellent detection capabilities.
What the New Perovskite Camera Achieved
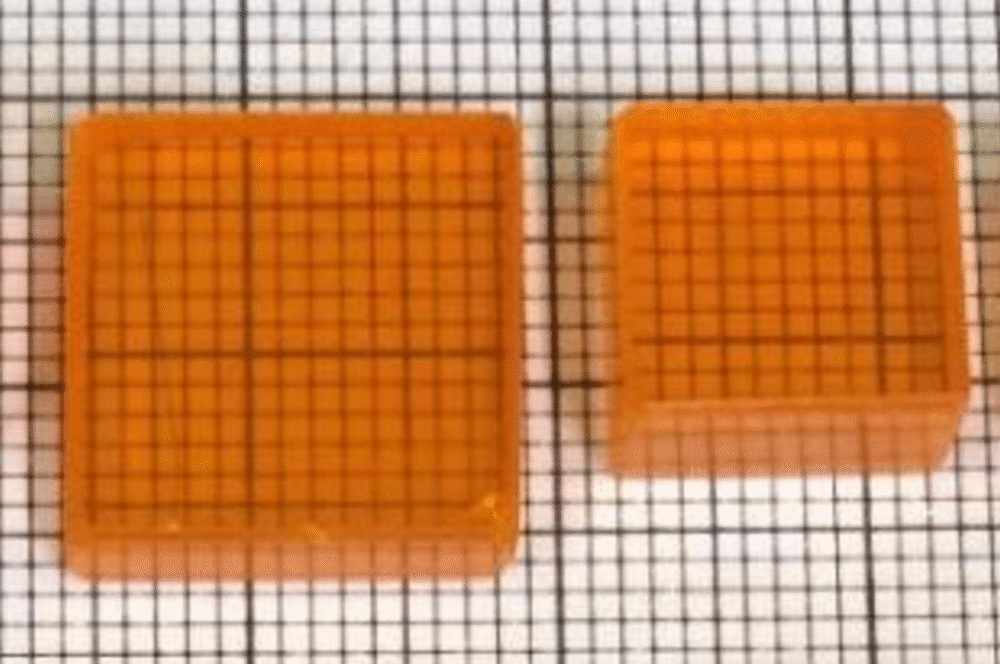
The team led by Mercouri Kanatzidis from Northwestern and Yihui He from Soochow University has successfully built and tested a prototype perovskite gamma-ray detector specifically for nuclear medicine imaging.
Here are the key technical achievements:
- Material Used: The detector is based on CsPbBr₃ perovskite single crystals.
- Design: They engineered a pixelated detector architecture, similar to the way smartphone cameras use pixels to capture images.
- Surface Engineering: The team applied chemical-mechanical polishing to reduce charge loss on the crystal’s surface, which dramatically improved efficiency, stability, and image clarity.
- Energy Resolution:
- 2.5% at 141 keV, the gamma energy emitted by technetium-99m (the most commonly used SPECT radiotracer).
- 1.0% at 662 keV, typical of a cesium-137 source.
- Sensitivity: The system demonstrated high sensitivity, between 0.13%–0.21% counts per second per becquerel (cps/Bq).
- Spatial Resolution: In phantom tests, the detector could clearly separate sources just 7 mm apart, corresponding to a sharp resolution of about 3.2 mm.
- Stability: The detector remained stable during extended tests, with minimal signal loss or distortion.
All of these numbers are either on par with or better than the best CZT detectors currently used in hospitals, and far better than sodium iodide detectors.
Why This Matters for Patients
For patients, the advantages are immediate and practical:
- Shorter Scans: Because the detector is more sensitive, scans could be completed in less time.
- Lower Radiation Exposure: Patients may require smaller doses of radioactive tracers, reducing health risks.
- Sharper Images: Doctors can see clearer images, leading to more accurate diagnoses.
- More Access: Hospitals and clinics that couldn’t afford CZT-based cameras might finally have access to cutting-edge nuclear imaging.
This means better care not just for patients in big research hospitals, but also in community clinics and developing countries.
Commercialization and Next Steps
Northwestern has already spun out a company, Actinia Inc., to commercialize this technology. The goal is to scale up production of perovskite detectors, integrate them with practical imaging systems, and work with medical device companies to bring them into hospitals.
The fact that perovskites are easier to grow than CZT, and that the devices use simpler components, makes this commercialization pathway realistic. If successful, it could lead to widespread adoption in the next generation of SPECT and other nuclear medicine imaging devices.
Challenges Ahead
As with any new technology, there are challenges that need to be solved before perovskite detectors become mainstream:
- Mass Production: Scaling up crystal growth while maintaining consistent quality.
- Long-Term Stability: Ensuring that the detectors don’t degrade under continuous radiation exposure.
- Integration: Adapting the detectors into full imaging systems with multi-channel readouts and robust electronics.
- Regulatory Approval: Medical devices undergo rigorous safety and effectiveness testing before they can be used on patients.
Still, given the performance demonstrated in this study, many researchers believe these challenges are surmountable.
Extra Background: How SPECT Imaging Works
To appreciate this breakthrough, let’s take a quick look at how SPECT scans work.
- A patient is injected with a small dose of a radiotracer (often technetium-99m).
- The tracer emits gamma rays as it travels through the body.
- The detector (gamma camera) rotates around the patient, capturing these emissions.
- Each gamma ray is recorded as a data point, and millions of them are compiled to reconstruct a 3D image.
The sharper and more sensitive the detector, the better the resulting image. That’s why improving detector technology is such a big deal—it directly improves the quality of medical care.
Extra Background: What Are Perovskites?
Perovskites are a class of materials with a specific crystal structure named after the mineral calcium titanium oxide (CaTiO₃). What makes them special is their versatility:
- They can be engineered to conduct electricity, absorb light, or act as semiconductors.
- They have already revolutionized solar cells, offering cheap and efficient alternatives to traditional silicon.
- They are now being explored for LEDs, lasers, photodetectors, and radiation detectors.
The fact that the same class of materials can both harvest sunlight and detect gamma rays shows just how versatile and powerful perovskites really are.
Global Significance
High-quality nuclear imaging should not be a privilege limited to wealthy hospitals. By lowering costs and improving quality, perovskite detectors could open access to advanced diagnostics worldwide.
This breakthrough has been supported by multiple institutions, including the Defense Threat Reduction Agency, the National Key R&D Program of China, the National Natural Science Foundation of China, and the Jiangsu Natural Science Foundation. The collaboration highlights how international science partnerships can lead to innovations that benefit everyone.
Final Thoughts
The development of the world’s first perovskite gamma-ray camera is a milestone in both medical imaging and materials science. It shows that perovskites, once famous only for solar energy, can now bring about a revolution in nuclear medicine.
With sharper images, shorter scans, lower doses, and cheaper devices, this innovation could help millions of patients worldwide get better diagnoses and better care. The next steps will involve scaling up production, ensuring stability, and working through the long process of commercialization. But the foundation is solid: the perovskite camera works, and it works better than many of the detectors currently in use.
If successful, this could be the beginning of a new era in medical imaging—an era where clearer, faster, safer scans are available to more people, in more places, than ever before.