Junk DNA Offers a Surprising New Path for Treating Hard-to-Treat Blood Cancers

Researchers from King’s College London have revealed a fascinating and unexpected discovery that could change how we think about treating some of the toughest blood cancers. What was once dismissed as “junk DNA” is now being seen as a hidden weakness in cancer cells—one that existing drugs may be able to exploit. This finding opens up new opportunities for patients with limited treatment options, especially those with myelodysplastic syndrome (MDS) and chronic lymphocytic leukemia (CLL).
In this article, we’ll break down the research in detail: what was discovered, why it matters, how the experiments were done, and what it might mean for the future of cancer treatment. Along the way, we’ll also dive into some extra background about junk DNA, transposable elements, and PARP inhibitors, so that you’ll walk away with not just the news but also a deeper understanding of the science behind it.
The Challenge of Treating Certain Blood Cancers
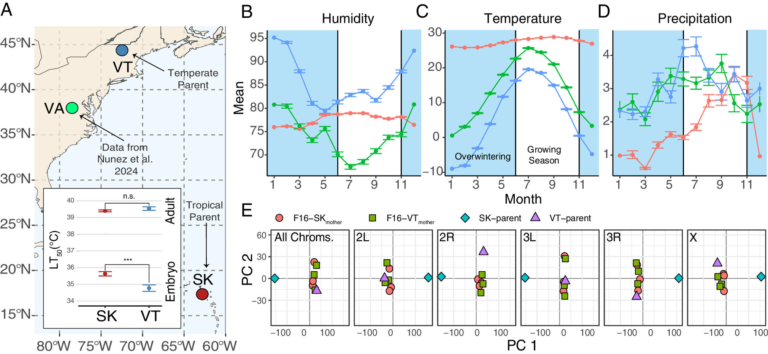
Blood cancers like MDS and CLL often involve mutations in two genes called ASXL1 and EZH2. These genes normally act as regulators, making sure other genes are properly switched on or off. When mutations disrupt their function, cells lose control over normal growth, leading to the uncontrolled spread of abnormal cells.
Here’s the problem: traditional cancer treatments usually target harmful proteins produced by defective genes. But in the case of ASXL1 and EZH2, the mutations often remove the protein entirely. With nothing left to inhibit, the usual drug approaches don’t work. This leaves patients with fewer treatment options and typically worse outcomes.
From Junk DNA to Therapeutic Target
About half of the human genome is made up of repetitive DNA sequences known as transposable elements (TEs). For decades, these were dismissed as useless genetic clutter—hence the nickname junk DNA.
But the King’s College London team showed that in cancers with ASXL1 and EZH2 mutations, these TEs become unusually active. When activated, they can move around in the genome, causing DNA breaks and instability. This puts enormous stress on cancer cells and makes them vulnerable to further DNA damage.
The beauty of this finding is that it transforms what was thought to be irrelevant genetic material into a therapeutic opportunity.
Repurposing PARP Inhibitors
The real breakthrough came when researchers tested PARP inhibitors, a class of drugs already used in treating certain cancers like ovarian and breast cancers.
Normally, PARP inhibitors work by blocking a DNA repair process that cancer cells rely on when they have specific mutations, such as those in BRCA1/BRCA2. But in this case, they operated differently.
Here’s what happens:
- When TEs jump around in the genome, they cause DNA breaks.
- Usually, PARP proteins repair this damage and keep the cancer cell alive.
- Blocking PARP with inhibitors means the damage piles up, eventually killing the cancer cell.
This is a completely new mechanism for PARP inhibitors. Instead of working through BRCA-related pathways, they exploit the TE activity triggered by ASXL1 and EZH2 mutations.
Confirming the Mechanism with Reverse Transcriptase Inhibitors
To make sure this wasn’t just coincidence, the scientists used reverse transcriptase inhibitors—drugs that stop TEs from copying themselves. When these were applied, the effect of the PARP inhibitors disappeared.
This confirmed that the killing power of PARP inhibitors in these cancers was indeed tied to transposable elements, not their typical role in other cancers.
Wider Impact for Cancer Therapy
This discovery doesn’t just apply to MDS and CLL. Other cancers with similar loss-of-function mutations in gene regulators could also show the same vulnerability. That means PARP inhibitors—already available and approved—could potentially be repurposed for a whole new range of cancers.
Of course, more work is needed. Clinical trials will be essential to test safety, dosing, and long-term effectiveness. But the fact that the drugs are already on the market makes the path to translation much faster.
What Are Transposable Elements?
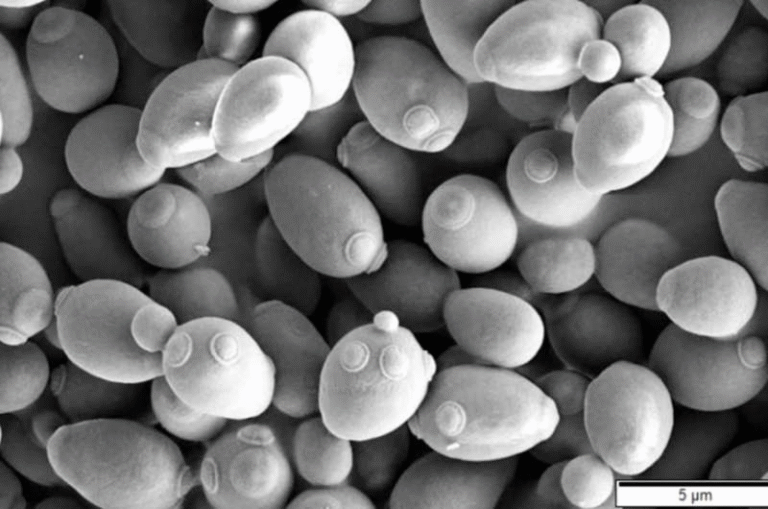
To fully appreciate this finding, let’s take a closer look at transposable elements (TEs). These are pieces of DNA that can move around the genome, sometimes called “jumping genes.”
There are two main types:
- Retrotransposons – These copy themselves via an RNA intermediate, similar to how some viruses replicate.
- DNA transposons – These move directly from one spot to another in the DNA.
While TEs can create genetic diversity, their uncontrolled activity can also be dangerous, leading to mutations and DNA damage. That’s why our cells normally keep them tightly suppressed.
The discovery that cancer mutations can reactivate these elements shows just how much junk DNA is tied into essential cellular processes.
What Are PARP Inhibitors?
PARP inhibitors (PARPi) are drugs that block Poly (ADP-ribose) polymerase (PARP) proteins. PARP proteins help repair DNA damage in cells.
In cancers with DNA repair deficiencies (like BRCA mutations), blocking PARP overwhelms the cell, leading to cell death. This concept is known as synthetic lethality, where two defects together (one genetic, one drug-induced) kill the cell, even though either alone might not.
The novelty in this research is that synthetic lethality is now achieved not through BRCA mutations, but through TE activity caused by ASXL1 and EZH2 mutations.
Experimental Evidence Behind the Discovery
The researchers provided strong evidence using several approaches:
- Mouse models with ASXL1 and EZH2 mutations showed TE reactivation, DNA damage, and sensitivity to PARP inhibitors.
- Human patient samples from MDS and CLL also showed the same vulnerability.
- Adding reverse transcriptase inhibitors reversed the effect, proving the link to TEs.
- In live animals, PARP inhibitors extended survival and reduced disease symptoms.
This multi-level evidence makes the finding especially compelling.
Why This Matters Beyond Blood Cancers
The broader implication is that cancers caused by loss of regulatory gene function may be targeted in ways we never thought possible. Instead of searching endlessly for new drugs, scientists can sometimes find new ways to use existing drugs.
This research also highlights the need to look deeper into what we once thought was irrelevant DNA. Half of our genome is made up of TEs, and this study shows that ignoring them could mean missing critical opportunities.
The Road Ahead
While the study is exciting, there are still questions:
- How can doctors identify which patients have TE activation strong enough to respond to PARP inhibitors?
- Will cancers develop resistance over time, as they often do with other therapies?
- Could combining PARP inhibitors with other drugs make the effect stronger?
Answering these will take more studies and eventually clinical trials, but the potential is real.
A Bigger Picture: Junk DNA Is Not Junk
This discovery adds to a growing body of research showing that junk DNA isn’t junk at all. For decades, scientists assumed that repetitive DNA sequences had no purpose. But in recent years, TEs have been linked to:
- Early development, where they help regulate gene expression.
- Immune responses, where some TEs can trigger antiviral defenses.
- Brain function, where TE activity may contribute to diversity among neurons.
Now, with this cancer link, it’s clearer than ever that so-called junk DNA is actually a crucial part of biology.
Conclusion
The King’s College London study has turned an old assumption upside down. What was once dismissed as genetic garbage may actually hold the key to treating blood cancers that have resisted standard therapies. By revealing a new vulnerability tied to transposable elements and showing how existing drugs like PARP inhibitors can exploit it, the research opens a fresh path in cancer treatment.
It’s a reminder that the answers to today’s toughest medical problems may be hiding in the parts of biology we least expect.
Research Reference:
Transposable elements as novel therapeutic targets for PARPi-induced synthetic lethality in PcG-mutated blood cancer – Blood, 11 September 2025