Stem Cells Reverse Stroke Damage in Mice – A Major Step Toward Brain Regeneration
A new study by scientists at the University of Zurich (UZH) and the University of Southern California (USC) has revealed that stem cell therapy can reverse stroke damage in mice, restoring both brain structure and motor function. This breakthrough brings researchers one step closer to regenerative treatments for stroke and other brain injuries that are currently considered irreversible.
What Happens During a Stroke
A stroke occurs when the blood flow to a part of the brain is cut off, depriving brain cells of oxygen and nutrients. Within minutes, neurons begin to die, causing lasting damage. Depending on the location and severity, patients can lose the ability to move, speak, or even think clearly.
Globally, about one in four adults will experience a stroke in their lifetime, and nearly half of those survivors are left with some form of permanent impairment. Modern medicine can manage symptoms and reduce risk factors, but there is still no therapy that repairs the dead brain tissue itself.
That’s what makes this new study remarkable—it shows real evidence of neural tissue regeneration after a stroke.
The Study: How Scientists Repaired the Brain
The team led by Christian Tackenberg and Rebecca Weber at UZH’s Institute for Regenerative Medicine, in collaboration with Ruslan Rust at USC, designed two complementary studies to test whether human neural stem cells could help regrow damaged brain tissue.
These weren’t just any stem cells. The researchers used induced pluripotent stem cells (iPSCs)—cells reprogrammed from normal human somatic (body) cells. iPSCs can be coaxed into becoming neural stem cells, which in turn can develop into neurons and other types of brain cells.
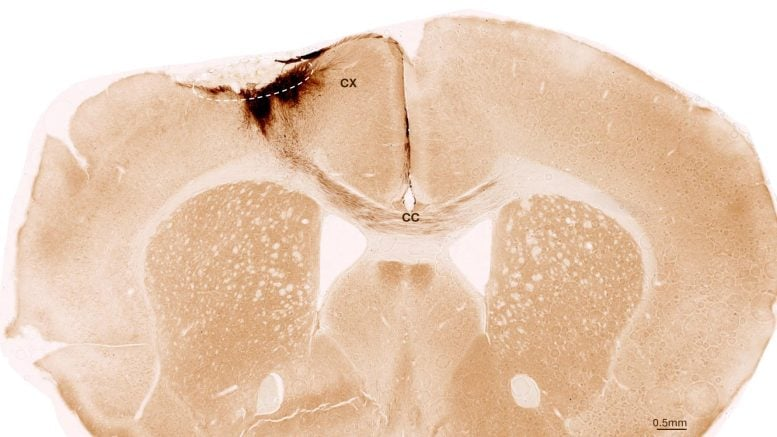
In the experiment, scientists first induced a permanent stroke in mice, replicating how strokes occur in humans. The animals were genetically modified to avoid rejecting human cells, ensuring the transplanted stem cells could survive and integrate.
One week after the stroke, the researchers transplanted human neural stem cells directly into the damaged region of the mouse brain. The team then observed the mice for the next five weeks, using imaging, biochemical analyses, and even AI-assisted behavioral tests to track changes.
The Results: Stem Cells That Became Neurons
The results were astonishing. The transplanted stem cells survived the entire observation period and transformed primarily into neurons, rather than support cells. More importantly, these new neurons connected with the mice’s existing brain cells, forming communication pathways similar to natural brain circuits.
This wasn’t just a visual observation—scientists verified neural activity and signaling between the transplanted cells and the host neurons. These new neurons weren’t passive passengers; they were actively integrating and helping rebuild damaged connections.
Regeneration Beyond Neurons
The benefits didn’t stop at neuron replacement. Researchers found that the stem cell transplants also triggered several other regenerative processes across the brain:
- New blood vessel formation (angiogenesis), improving oxygen and nutrient supply.
- Reduction in inflammation, which usually worsens brain injury after a stroke.
- Restoration of the blood-brain barrier, a crucial layer that protects the brain from harmful substances.
- Stimulation of the brain’s own repair mechanisms, encouraging native cells to regenerate.
This multi-layered recovery is what sets the study apart from previous work. Instead of merely replacing lost neurons, the transplanted stem cells seemed to kickstart the brain’s overall healing environment.
Functional Recovery Confirmed
The true test came in assessing whether these structural improvements translated into functional recovery. Using a specialized AI-based gait analysis system, scientists analyzed how the mice walked and moved after the stroke and transplantation.
The mice that received stem cells regained much of their motor coordination and limb movement, performing significantly better than those without transplants. The AI system picked up even subtle improvements that were difficult to detect by eye.
This kind of recovery is particularly encouraging because it suggests that the new neurons were successfully wired into the brain’s existing control networks, allowing normal movement to resume.
The Perfect Timing for Transplantation
One of the most surprising findings was that delayed transplantation worked better than immediate intervention.
Traditionally, it’s assumed that earlier treatment leads to better recovery. However, the UZH and USC teams found that waiting about a week after a stroke before performing the transplant yielded the best results.
This delay likely allows the brain to stabilize from the initial injury and inflammation, creating a more receptive environment for the new cells to grow. Clinically, this discovery is crucial—it means that patients wouldn’t need surgery in the chaotic hours after a stroke. Doctors could have a realistic treatment window of several days, making the therapy much more practical.
Preparing for Human Applications
While this success in mice is a major milestone, the researchers are already planning for the future. Tackenberg and his colleagues designed their stem cells without using any animal-derived substances, a critical step for human clinical applications. The protocol was developed in collaboration with the Center for iPS Cell Research and Application (CiRA) at Kyoto University.
The team is also working on several safety improvements. One focus is a “safety switch” system, which would allow doctors to deactivate transplanted cells if they begin to grow uncontrollably—a vital safeguard against tumor formation.
In parallel, scientists are exploring less invasive delivery methods, such as endovascular injection through blood vessels, instead of direct brain surgery. This approach could make the therapy safer and easier for patients.
Tackenberg’s group notes that similar stem cell treatments are already being tested in humans for Parkinson’s disease in Japan. Stroke, given its global prevalence, could be the next major target for clinical trials.
The Science Behind Stem Cell-Based Brain Repair
To understand why these results are so groundbreaking, it helps to know how neural stem cells work. These cells are capable of both self-renewal (making more stem cells) and differentiation (becoming specialized brain cells like neurons or astrocytes).
In a damaged brain, stem cells can serve two major purposes:
- Cell replacement – they physically replace dead or dying neurons.
- Neuroprotection and modulation – they release growth factors and signals that help the surviving neurons recover.
In this study, both effects were observed. The transplanted cells didn’t just sit there; they communicated with the host brain via molecular crosstalk. Key signaling pathways, including neurexin, neuregulin, NCAM, and SLIT, were found to be active between grafted and native cells. These molecular interactions seem to guide the integration of new neurons and the reorganization of neural circuits.
This crosstalk might be one of the missing pieces in understanding why some stem cell therapies work better than others—it’s not only about replacing lost cells but also about reprogramming the brain’s healing response.
Challenges Still Ahead
Despite the promising outcomes, several challenges remain before this therapy can reach hospitals. Translating from mice to humans is a complex task. Human strokes often affect much larger brain areas and involve additional factors such as age, co-existing diseases, and variable immune responses.
Long-term monitoring is also essential. The study observed mice for five weeks, which is significant in animal research but still short compared to human recovery timelines. Scientists will need to confirm that these effects last for months or even years, and that the new neurons remain functional and stable.
Finally, the question of scale arises—how to generate and deliver enough safe, high-quality stem cells for human patients on a large scale.
Broader Impact on Neuroscience and Medicine
This study adds momentum to a growing field of regenerative neuroscience, where researchers aim not just to treat but to restore the brain. Over the past decade, progress in induced pluripotent stem cell technology has opened possibilities for personalized cell-based therapies, where a patient’s own skin or blood cells could be converted into neural stem cells for transplantation.
Similar approaches are already under clinical evaluation for Parkinson’s disease, spinal cord injuries, and retinal degeneration. The success of this stroke study strengthens the case for stem cell-based brain repair more broadly.
If the next steps in safety and scaling succeed, it could mark the beginning of a new era in treating neurological diseases—one where lost brain function is not just managed but actually rebuilt.
Why This Research Matters
Every year, around 12 million people worldwide experience a stroke. For many survivors, recovery plateaus after a few months, leaving them permanently disabled. Current rehabilitation methods can help patients regain partial function but cannot replace dead neurons.
This new study suggests that might one day change. By demonstrating that human-derived stem cells can form real, functioning neural connections in a damaged brain, researchers have opened a pathway toward therapies that could restore movement, cognition, and independence to millions.
It’s a cautious optimism, but it’s backed by strong data and careful methodology. The road to human trials may be long, but the direction is clearer than ever before.