New Study Raises Concerns: Is the “Safe” Pregnancy Pill (Acetaminophen) Really So Safe?
A major new review report suggests that prenatal exposure to acetaminophen (also known as paracetamol, and in the U.S. as Tylenol®) may be linked with higher risks of autism and ADHD in children.
The authors use a rigorous evaluation method and call for serious reconsideration of clinical guidelines. At the same time, leading medical groups caution that this is not proof of causation and stress the importance of balanced decision-making. In this article, I’ll lay out all the concrete details of the study, the responses from health authorities, the strengths and limitations, and extra background knowledge you might find useful.
What the Study Did and What It Found
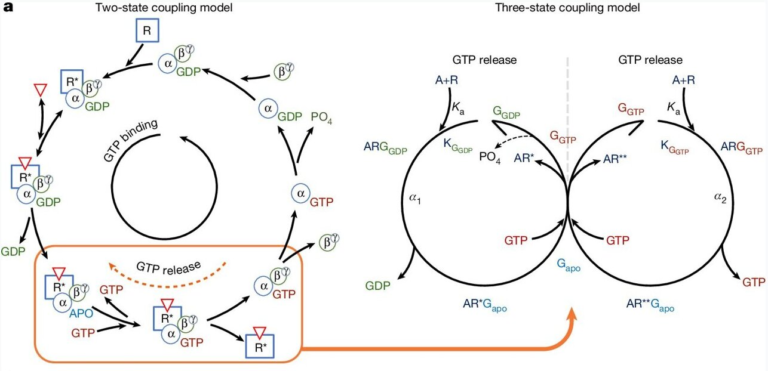
A Systematic Review with the Navigation Guide Method
Researchers led by the Icahn School of Medicine at Mount Sinai applied the Navigation Guide methodology—a systematic, structured framework commonly used in environmental health—to analyze existing human studies on acetaminophen exposure in utero and neurodevelopmental outcomes. (BioMed Central)
Key points:
- The literature search was conducted through February 25, 2025, using PubMed and other sources. (ResearchGate)
- They identified 46 individual human studies that met inclusion criteria (excluding animal, in vitro, reviews, meta-analyses, etc.). (ResearchGate)
- Because of substantial heterogeneity (differences in how exposures and outcomes were measured, populations, study quality), the authors did not perform a quantitative meta-analysis. Instead, they opted for a qualitative synthesis, guided by Navigation Guide ratings of risk of bias and evidence strength. (ResearchGate)
From those 46 studies:
- 27 reported positive associations (i.e. statistically significant links between prenatal acetaminophen and neurodevelopmental disorders)
- 9 reported null associations (no significant link)
- 4 reported negative (protective) associations
- The remaining showed mixed or inconclusive results
- Importantly, the authors note that higher-quality studies—those with lower risk of bias—were more likely to show a positive association. (ResearchGate)
Thus, their summary conclusion is that the weight of evidence is consistent with an association between prenatal acetaminophen exposure and higher incidence of neurodevelopmental disorders (NDDs) in offspring, especially autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD). (ResearchGate)
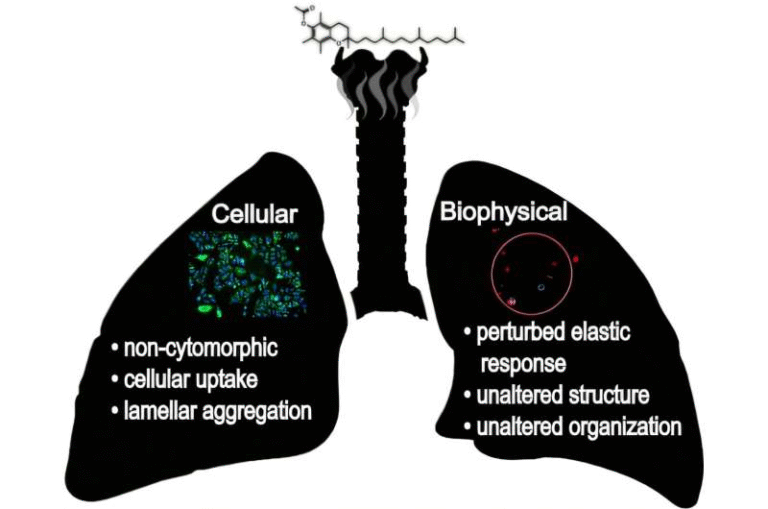
What Mechanisms Are Proposed?
The authors discuss several potential biological pathways—none proven in humans, but plausible in theory:
- Acetaminophen can cross the placental barrier and reach the fetus. (BioMed Central)
- It may induce oxidative stress in developing neural tissues
- It could disrupt hormone signaling (endocrine effects)
- It might trigger epigenetic changes (altering gene regulation) during critical windows of brain development
- These disruptions might interfere with neuronal growth, connectivity, or differentiation in the fetal brain
Because many brain developmental processes occur in utero in sequences and time windows, interventions or exposures that alter cellular balance at the wrong moment can have downstream, cascading effects (in theory). The authors emphasize that these mechanisms remain speculative and need further validation. (BioMed Central)
Practical Recommendations from the Authors
Given their findings, the authors make clear recommendations (with caution):
- Use acetaminophen in pregnancy only under medical supervision
- Prefer the lowest effective dose and the shortest possible duration
- Update clinical guidelines to more carefully balance benefits (e.g. treating fever or pain) and possible risks
- Further research is urgently needed—including better exposure measurement, prospective studies, and mechanistic work
- They emphasize not to stop medications abruptly without consulting a clinician, because untreated pain or fever itself may pose risks to the mother and baby
In short: this is not a call for elimination of acetaminophen in pregnancy, but for greater caution and more informed, evidence-driven guidance. (BioMed Central)
Mount Sinai has publicly summarized the study, noting that acetaminophen is used by more than half of pregnant women globally, and that applying the Navigation Guide is a first in this field. (Mount Sinai Health System)
Responses from Authorities & Experts
The new review stirred reactions from major medical and regulatory bodies. Here’s how they responded:
U.S. Food and Drug Administration (FDA)
- On September 22, 2025, the FDA announced it would initiate a label change for acetaminophen products (Tylenol and generics) to reflect possible associations with autism and ADHD. (U.S. Food and Drug Administration)
- The FDA also issued a Notice to Physicians advising that chronic use of acetaminophen—especially from pregnancy through delivery—may carry the greatest risk. (U.S. Food and Drug Administration)
- They emphasized that association ≠ causation—there is no conclusive proof that acetaminophen causes neurodevelopmental disorders. (U.S. Food and Drug Administration)
- The agency also pointed out that acetaminophen remains the only over-the-counter analgesic/antipyretic considered reasonably safe in pregnancy (compared to aspirin or ibuprofen, which have known fetal risks). (U.S. Food and Drug Administration)
- The FDA said it would notify physicians nationwide to balance risks and benefits, advising caution especially for routine, prolonged use in low-grade fever cases. (U.S. Food and Drug Administration)
Professional Medical & Obstetric Organizations
- ACOG (American College of Obstetricians and Gynecologists) reaffirmed that acetaminophen remains the analgesic/antipyretic of choice in pregnancy, when used judiciously. They caution that suggestions of a causal link are “not backed by the full body of scientific evidence.” (ACOG)
- ACOG urges that clinicians offer evidence-based counseling, reassure patients, and maintain access to acetaminophen in prenatal care. (ACOG)
- Additional statements from SMFM (Society for Maternal–Fetal Medicine) and FIGO (International Federation of Gynecology and Obstetrics) emphasize that current evidence does not support a causal link and stress caution in making sweeping policy changes. (ACOG)
Other Perspectives & Cautions
- Some commentators note that one of the study’s authors, Dr. Andrea Baccarelli, has served as an expert witness in lawsuits alleging links between acetaminophen and neurodevelopmental harm—a fact disclosed in the paper as a potential conflict of interest. (BioMed Central)
- Critics point to a large Swedish population cohort study (published in JAMA in 2024) of 2.48 million children which used sibling matched control analyses to adjust for familial confounding. That study found no evidence of increased risk of ASD, ADHD, or intellectual disability in sibling comparisons (hazard ratios ~0.98). (JAMA Network)
- That Swedish study suggests that previously observed associations may arise from shared family factors (genetics, environment, underlying maternal health). (JAMA Network)
- Media and fact-checkers are actively clarifying that no definitive proof exists that acetaminophen causes autism, and that discontinuing its use indiscriminately may be harmful (given the risks of untreated fever or pain). (PBS)
- Some debate is already emerging over whether the federal health announcement is political messaging rather than evidence-based medicine. (Reuters)
Strengths, Limitations, and Uncertainties
When interpreting all this, it helps to be crystal clear about what we know and what we don’t yet know.
Strengths of the New Review
- The use of the Navigation Guide gives structure and transparency to bias ratings, strength-of-evidence judgments, and synthesis strategy—not a mere narrative review.
- Inclusion of a relatively large number of human observational studies (46) across multiple countries.
- Careful attention to study quality: finding that higher-quality studies more often show positive associations is suggestive.
- Explicit acknowledgment of heterogeneity and limitation—no overclaiming of causation.
Key Limitations & Uncertainties
- Observational data only: there are no randomized trials testing acetaminophen vs. placebo for brain outcomes.
- Heterogeneity across studies: different exposure measures (self-report, registry, biomarkers), dosages, timing, outcome definitions, adjustment variables, populations.
- Confounding by indication: women may take acetaminophen due to fever, pain, infection, or other illnesses; those conditions themselves may influence fetal neurodevelopment.
- Familial confounding: shared genetic or environmental factors may explain associations—something sibling studies attempt to control for.
- Conflict of interest disclosures (e.g. authors working in legal settings) require cautious interpretation.
- Mechanisms are speculative in humans—not yet established.
- The absence of a pooled estimated effect size means we have no single quantitative risk estimate (e.g. “X% increase in autism risk per dose”).
Because of these limitations, one must not leap from association to causation. The authors and various medical bodies emphasize precisely that at length.
Broader Context & What You Should Know
To help you better situate this news, here are a few extra points and context you may find useful.
Why Acetaminophen Is Widely Used in Pregnancy
- Among over-the-counter pain relievers, acetaminophen is generally considered the safest choice in pregnancy (compared to aspirin or NSAIDs, which carry known fetal risks). (ACOG)
- It’s inexpensive, accessible, and over half of expectant mothers reportedly use it at some point during pregnancy. (BioMed Central)
- Fever in pregnancy, if unmanaged, can itself pose risks (to both mother and fetus). Some headaches or painful conditions are severe, and untreated pain is not innocuous.
What the Swedish Sibling Study Adds
- In the JAMA 2024 study, 2.48 million children born in Sweden between 1995 and 2019 were followed. (JAMA Network)
- In models without sibling comparisons, acetaminophen use was associated with small increases in risk (e.g. HR ~1.05 for autism, ~1.07 for ADHD). (JAMA Network)
- But when comparing within sibling pairs (i.e. controlling for shared genes and family environment), no significant associations remained (HR ~0.98 for both autism and ADHD). (JAMA Network)
- This suggests that shared familial factors may explain much of the apparent association seen in observational cohorts.
The Legal & Social Backdrop
- There is already a mass tort / litigation backdrop in the U.S., where lawsuits claim that acetaminophen during pregnancy caused autism or ADHD in children. (Wikipedia)
- Some courts have pushed back, criticizing the plaintiffs’ expert arguments as cherry-picking data and overinterpreting weak associations. (Wikipedia)
- Because this issue has public visibility, health agencies and medical societies are under pressure to respond carefully—but also quickly.
What Should Pregnant Women & Clinicians Think Now?
Given all the above evidence, here’s a reasoned, cautious approach (which is basically what leading organizations are recommending):
- Don’t panic and stop all acetaminophen use. Doing so without medical guidance may expose mother and fetus to risks from untreated pain or fever.
- When using acetaminophen, opt for the lowest effective dose and limit duration (i.e. avoid chronic daily use when not necessary).
- Always discuss medication use with your obstetrician or healthcare provider, especially if you have frequent pain or fever during pregnancy.
- Clinicians and guideline committees should review recommendations in light of emerging evidence, but avoid making sweeping changes prematurely.
- Watch carefully for future research—especially prospective cohorts, stronger exposure measurement, and mechanistic human studies.
In short: this is a caution-raising study, not a guarantee of harm. It invites us to re-examine what was considered “safe by default” and to demand better evidence.
Here is the research paper that the review is based on:
Diddier Prada, Beate Ritz, Ann Z. Bauer & Andrea A. Baccarelli. “Evaluation of the evidence on acetaminophen use and neurodevelopmental disorders using the Navigation Guide methodology.” Environmental Health. DOI: 10.1186/s12940-025-01208-0 (Open access) (BioMed Central)