MIT and Harvard Scientists Create “Invisible” Immune Cells That Obliterate Cancer Without Being Detected
A new study from MIT and Harvard Medical School has unveiled a groundbreaking step forward in cancer immunotherapy. Scientists have successfully engineered CAR-NK cells — special immune cells that can both evade immune detection and destroy cancer cells with remarkable precision. These modified natural killer (NK) cells were tested in humanized mice, where they effectively wiped out cancer while avoiding the dangerous immune reactions that often plague cell-based therapies.
This research, published on October 8, 2025, in Nature Communications, introduces a method to make “off-the-shelf” immune cells that don’t need to come from each patient individually. This means faster treatments, potentially safer outcomes, and a significant leap toward making personalized cancer therapy more accessible.
What Exactly Are CAR-NK Cells?
To understand why this discovery matters, it’s helpful to know what NK cells and CAR-NK cells are.
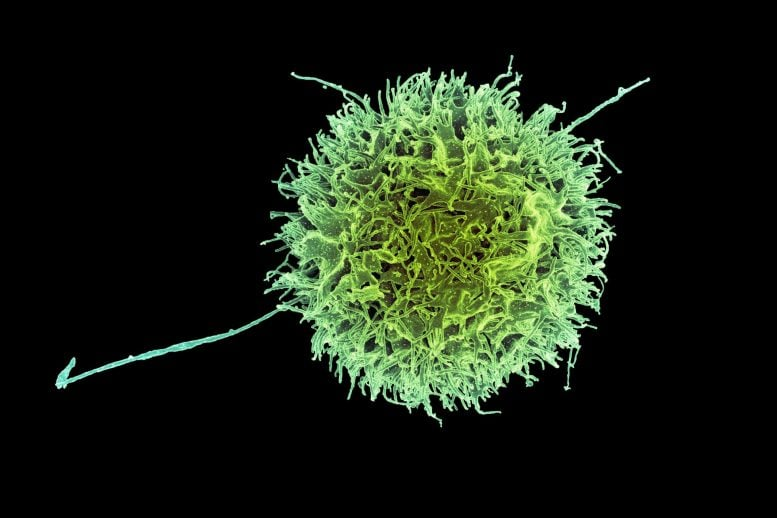
Natural Killer (NK) cells are a vital part of our body’s immune defense. They act like patrol units that recognize and eliminate virus-infected cells or cancerous cells. Unlike T cells, NK cells don’t require prior exposure to their targets. They can identify and kill dangerous cells using several methods, one of which is called degranulation — releasing proteins such as perforin that punch holes in target cells, leading to their destruction.
CAR-NK cells take this natural power and enhance it with genetic engineering. Scientists add a Chimeric Antigen Receptor (CAR) — a custom-built protein that helps NK cells specifically target certain cancer markers, like CD19, which is common on lymphoma cells. This engineering makes NK cells more precise and lethal against cancer.
While this approach is similar to CAR-T cell therapy, which has already shown major success against blood cancers, CAR-NK therapy has potential advantages. NK cells are naturally less likely to trigger life-threatening side effects like cytokine release syndrome (CRS) and neurotoxicity, which sometimes occur with CAR-T treatments.
The Problem: Immune Rejection
Despite their potential, CAR-NK treatments face a huge obstacle — immune rejection.
Typically, a patient’s own NK cells are extracted, genetically modified, and then multiplied in a lab before being infused back into their body. This process takes several weeks and isn’t always successful, especially in patients with weakened immune systems.
To overcome that, researchers have long dreamed of using donor NK cells from healthy people. These could be mass-produced and stored, ready to use immediately after a cancer diagnosis. However, donor cells often don’t last long in the body. The patient’s immune system quickly identifies them as “foreign” because they carry HLA class I proteins — molecules that vary between individuals and serve as cellular ID tags. When these HLAs don’t match, the patient’s immune system destroys the donor NK cells.
That’s the challenge the MIT-Harvard team set out to solve: How can we make donor NK cells invisible to the immune system?
The Engineering Breakthrough
The scientists, led by Jianzhu Chen of MIT’s Koch Institute and Rizwan Romee of Harvard Medical School and Dana-Farber Cancer Institute, designed a single genetic construct that introduces several coordinated modifications to NK cells all at once.
Here’s what they did:
- Knocked Down HLA Class I Proteins:
Using short interfering RNA (siRNA), the team suppressed the genes responsible for producing HLA class I proteins. Without these proteins, the NK cells become harder for T cells (a major component of the immune system) to recognize and attack. - Added PD-L1 Expression:
They engineered the cells to express PD-L1, a protein known for sending inhibitory signals to T cells. This helps the engineered NK cells calm down potential immune attacks from the host’s T cells, allowing them to survive longer. - Introduced Single-Chain HLA-E (SCE):
The researchers also added a version of HLA-E, called single-chain HLA-E or SCE. This protein interacts with receptors on other NK cells, preventing “friendly fire” from the patient’s own NK cells. Essentially, it tells them not to attack. - Inserted a CAR Gene Targeting CD19:
Finally, the scientists added a CAR gene designed to recognize CD19, a protein found on many B-cell cancers like lymphoma.
What’s particularly elegant about this method is that all of these elements — the CAR, the siRNA for HLA suppression, PD-L1, and SCE — are delivered using a single piece of DNA. This “one-step engineering” makes it simpler, faster, and more efficient to create immune-evasive CAR-NK cells.
Testing the Invisible Immune Cells
The researchers tested their newly engineered NK cells in humanized mice — mice with immune systems that mimic human biology — which were implanted with CD19-positive lymphoma cells.
The results were stunning.
- The engineered CAR-NK cells survived and thrived for over three weeks in the mice.
- They nearly eliminated all traces of cancer during this period.
- In contrast, control groups that received either unmodified NK cells or cells engineered only with the CAR gene (without the immune-evasion features) saw their NK cells die off within two weeks — and their cancers continued to grow unchecked.
Even more promising was the safety profile. The modified CAR-NK cells caused far less cytokine release syndrome, a common and dangerous side effect of immune-based cancer treatments. This suggests that the therapy could offer stronger results with fewer risks than existing CAR-T therapies.
Why This Matters
The implications of this research are massive.
First, it could make cancer immunotherapy much faster. Traditional CAR-T and CAR-NK therapies require weeks to harvest and engineer a patient’s own cells. With this new approach, pre-engineered donor cells could be stored and ready for immediate use — a true “off-the-shelf” cancer treatment.
Second, these cells appear to be safer and longer-lasting. By hiding from the host immune system, they remain active longer and can continue hunting down cancer cells without triggering dangerous inflammation.
Third, this could cut treatment costs dramatically. Personalized therapies are expensive and labor-intensive, but a standardized CAR-NK product could be produced at scale.
Who’s Behind the Work?
This research was a collaboration between MIT’s Koch Institute for Integrative Cancer Research, Harvard Medical School, and the Dana-Farber Cancer Institute.
Lead contributors include Fuguo Liu, a postdoctoral researcher at the Koch Institute and Dana-Farber, and senior authors Jianzhu Chen and Rizwan Romee.
The project was funded by several organizations, including Skyline Therapeutics, the Koch Institute Frontier Research Program, the Claudia Adams Barr Foundation, and the National Cancer Institute through the Koch Institute Support Grant.
The Next Steps: From Mice to Humans
While the preclinical results in mice are extraordinary, translating them to humans is a major next step. The researchers plan to collaborate with clinicians at Dana-Farber to begin clinical trials.
They’re also partnering with a local biotech company to explore using similar immune-evasive NK cells for autoimmune diseases like lupus, where the immune system attacks healthy tissues. In that context, NK cells could be used to regulate and calm overactive immune responses rather than fight cancer.
If successful, this could represent not just a cancer breakthrough, but a new era in immune engineering — where cell therapies can be universally compatible, pre-manufactured, and precisely tuned for different diseases.
Understanding the Bigger Picture: The Rise of Cell-Based Immunotherapy
Immunotherapy has completely changed how doctors think about treating cancer. Instead of relying only on chemotherapy or radiation, these treatments empower the immune system to do the killing.
CAR-T cell therapy was the first big success story, earning FDA approvals for blood cancers like leukemia and lymphoma. However, CAR-T treatments are complex, costly, and sometimes dangerous. The engineered T cells can overreact, releasing a flood of inflammatory molecules that cause fever, low blood pressure, and organ damage.
That’s where CAR-NK cells come in. Unlike T cells, NK cells don’t rely on recognizing a specific foreign antigen through the T cell receptor. They naturally seek out “stressed” or “abnormal” cells, making them ideal for detecting cancer cells that may try to hide from other immune defenses.
In addition, NK cells don’t cause graft-versus-host disease (GVHD) — a severe complication where donor immune cells attack the recipient’s tissues. This makes them inherently safer for use across different individuals.
Researchers worldwide are now testing CAR-NK therapies for a variety of cancers, including acute myeloid leukemia (AML), multiple myeloma, and even some solid tumors like liver and lung cancers. There are now more than 120 CAR-NK trials ongoing globally, reflecting just how much potential this field has.
The Remaining Challenges
Despite all this progress, several hurdles remain before these invisible NK cells reach hospitals.
- Persistence: While three weeks of survival in mice is impressive, cancer in humans may require cells that persist for months. Scientists are working to find ways to keep CAR-NK cells alive longer without losing their potency.
- Manufacturing: Creating a multi-gene construct that includes CARs, siRNA, and regulatory proteins is technically demanding. Scaling it up for clinical use must ensure consistent quality and safety.
- Tumor Diversity: Cancers can evolve and lose the markers that CAR-NK cells target. Future designs might include multiple CARs or adaptable receptors to prevent tumor escape.
- Translation to Solid Tumors: Blood cancers are easier for immune cells to reach, but solid tumors present barriers like dense tissue and immunosuppressive environments. Overcoming that remains a tough challenge.
Still, this new MIT-Harvard study shows that immune invisibility can be engineered — and that’s a game-changer for all future cell therapies.