Caltech Researchers Use a Revived Imaging Technique to Reveal Hidden Secrets of Bacterial Biofilms
Bacterial biofilms—those dense, sticky communities of microbes that cling to surfaces—have long puzzled scientists because of their remarkable resilience. These structures, which can form on medical devices, tissues, and even in industrial pipelines, are notoriously tough to destroy. Now, researchers at the California Institute of Technology (Caltech) have reintroduced a classic imaging technique that provides an entirely new window into how these biofilms grow, organize, and defend themselves.
This study, led by postdoctoral researcher Georgia Squyres in the lab of Professor Dianne Newman, was recently published in the journal Proceedings of the National Academy of Sciences (PNAS). It not only revives an older microscopy approach but also modernizes it to study bacterial communities at an unprecedented level of detail. The results help explain how some bacteria resist antibiotics and how they manage to build strong, self-healing protective layers.
Understanding What Biofilms Are
Before diving into the study, it’s worth clarifying what a biofilm actually is. A biofilm is a dense, structured community of bacteria that stick together and to surfaces by secreting a slimy substance known as the extracellular matrix. This matrix acts as a kind of glue, holding the community together and protecting it from external threats such as antibiotics or immune system attacks.
Biofilms can form on a wide range of surfaces—catheters, wounds, teeth (as dental plaque), water pipes, or even rocks in rivers. Within these communities, bacteria behave differently from their free-swimming counterparts. They communicate, share nutrients, and even coordinate defense strategies.
One of the key reasons biofilms are medically important is that they are extremely tolerant to antibiotics. In some chronic infections, biofilms can survive doses of drugs that would normally kill free-floating bacteria. Understanding how these communities organize and protect themselves is therefore vital to finding better treatments.
The Problem with Imaging Biofilms
Imaging biofilms has always been a technical challenge. Traditional biological imaging methods often use fluorescent proteins to label and track cells. The issue is that these fluorescent markers require oxygen to function, and oxygen is scarce in the dense core of most biofilms. That means scientists could only see the outer layers, leaving the interior—where much of the interesting biology happens—largely invisible.
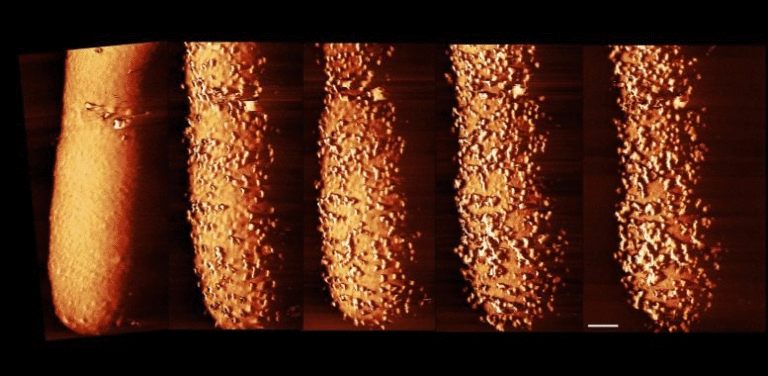
Squyres and her team needed a way to visualize every cell in the biofilm, even those in oxygen-deprived regions. To solve this, they brought back a classic contrast technique: instead of labeling the bacterial cells themselves, they labeled the medium (the material in which the cells grow) with a cheap, non-toxic dye. In this setup, the medium glows brightly while the cells appear dark against it.
This simple yet clever trick made it possible to see and track individual bacterial cells throughout the entire biofilm structure—even deep inside where oxygen levels drop to zero. It also allowed the researchers to observe the biofilm continuously for days at a time without damaging it.
Watching Biofilms Grow Cell by Cell
Using this imaging technique, the researchers observed biofilms of Pseudomonas aeruginosa, a bacterial species often responsible for hospital-acquired infections and known for forming stubborn biofilms. By combining the imaging with computer algorithms that could track individual cells, Squyres was able to monitor the growth, division, and death of bacteria over many days.
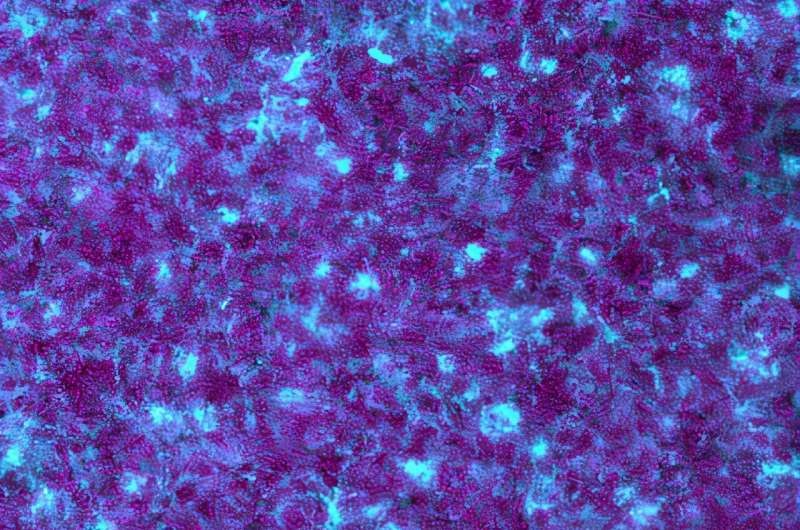
One of the most striking discoveries was the process of cell lysis—when a bacterial cell dies and bursts open. The team found that these lysis events weren’t random. Instead, only a small proportion of cells (roughly one in every 10,000 per hour) undergo lysis, and they do so in specific areas within the biofilm.
When these cells rupture, they release extracellular DNA (eDNA) into the matrix. This DNA acts like a building material, strengthening the biofilm’s structure and helping cells stick together. The eDNA also traps antibiotics, preventing them from reaching their bacterial targets. In other words, some cells in the biofilm effectively sacrifice themselves to reinforce the community’s defenses.
Mapping the Death and Defense Zones
By mapping where lysis occurred, Squyres noticed a fascinating pattern: these events happen in regions shaped by nutrient and oxygen gradients. Inside a biofilm, not all areas are equal—oxygen and carbon sources are more abundant near the surface and become scarce deeper inside. The cells that die tend to be located in specific layers defined by these gradients.
Introducing oxygen artificially into the oxygen-deprived core caused cells there to burst, confirming that oxygen levels influence the process. This suggests that bacteria within the biofilm are somehow able to sense and respond to local environmental conditions, organizing their own structure through controlled cell death.
Over time, the release of eDNA from lysed cells shapes the overall architecture of the biofilm, giving it both structural integrity and chemical protection. This intricate patterning explains how biofilms maintain a consistent shape and stability as they expand.
A Fresh Look at an Old Technique
The imaging method that Squyres reintroduced is elegant in its simplicity. By labeling the surrounding medium rather than the cells, she avoided the oxygen limitation problem that hinders fluorescent labeling. The dye used is cheap, safe, and effective, allowing for high-resolution, long-term imaging even in dense microbial communities.
This approach opens up possibilities far beyond just Pseudomonas aeruginosa. Any bacterial species that forms a biofilm could potentially be studied using this method. That includes pathogens associated with chronic infections, as well as environmental bacteria important for wastewater treatment or bioremediation.
Professor Dianne Newman, who supervised the work, emphasized that beyond the technical innovation, the true achievement lies in the ability to ask new kinds of biological questions—about how bacterial communities organize, evolve, and behave at the single-cell level over time.
Why This Research Matters
This work sheds light on how microbial communities self-organize, and it may help researchers design new strategies to combat biofilm-related infections. If scientists can figure out how to disrupt the patterns of cell death or the formation of eDNA, they might be able to weaken biofilms and make antibiotics more effective.
It also changes how we think about bacteria. Rather than being simple, individual organisms, the bacteria in a biofilm operate more like a multicellular organism—different cells performing different roles, some even dying to benefit the group. This kind of collective behavior challenges the traditional view of bacteria as solitary and simple life forms.
Beyond medicine, this knowledge could be useful in biotechnology and environmental engineering. Biofilms play roles in water treatment systems, corrosion processes, and natural ecosystems. Understanding how they develop could allow us to either enhance beneficial biofilms or prevent harmful ones.
The Bigger Picture on eDNA and Antibiotic Tolerance
The study also deepens our understanding of extracellular DNA, a major component of the biofilm matrix. eDNA doesn’t just provide structure—it also acts as a molecular sponge that traps antibiotics, enzymes, and signaling molecules. This is one reason why infections involving biofilms, such as chronic lung infections in cystic fibrosis patients, are so difficult to treat.
Researchers have long known that eDNA plays a role in biofilm stability, but this study finally shows how and where that DNA is produced and organized. The fact that patterned cell death drives this process adds a new layer of complexity to biofilm biology.
A Step Forward in Biofilm Research
The study by Georgia Squyres and Dianne Newman provides a clear, detailed picture of how bacterial communities self-organize their defenses. It combines a revived imaging method, careful quantitative analysis, and thoughtful biological interpretation to reveal how biofilms grow and persist.
The discovery that lysis events are patterned by metabolic gradients could have profound implications for microbiology, infectious disease research, and antibiotic therapy. It opens up a fresh line of investigation into how microbial societies manage life and death within their ranks—and how that coordination makes them so difficult to defeat.
For researchers working on chronic infections or bacterial resistance, this work offers not only new insights but also new experimental tools to explore life inside biofilms in real time.
Research Reference:
Single-cell lysis patterns morphogenesis of eDNA in the matrix of Pseudomonas aeruginosa biofilms, Proceedings of the National Academy of Sciences (2025)