New Lipid Nanoparticles Can Deliver mRNA Directly Into Heart Muscle Cells, Opening Doors for Future Cardiac Gene Therapies
A team of researchers from UC Berkeley, Gladstone Institutes, and UCSF has achieved a major step forward in gene therapy for heart disease. They’ve developed lipid nanoparticles (LNPs) capable of efficiently delivering messenger RNA (mRNA) directly into heart muscle cells, also known as cardiomyocytes. Their findings, published in Nature Biomedical Engineering, could mark the beginning of a new generation of treatments for heart failure and other cardiac disorders.
The Persistent Challenge of Treating the Heart
Cardiovascular diseases remain the world’s leading cause of death, yet progress in developing new heart treatments has slowed over the past decade. The key challenge has been delivering therapeutic molecules precisely to heart cells without causing damage or unwanted effects in other tissues. The heart’s dense structure, limited regenerative ability, and continuous motion make it a difficult organ to target.
Traditional treatments can manage symptoms but rarely address the root cellular or genetic causes of heart failure. Gene therapy and mRNA-based therapeutics—technologies that reprogram or repair cells from within—hold promise, but getting those genetic instructions into cardiomyocytes has been a persistent obstacle.
What Makes mRNA Therapy So Promising
Messenger RNA (mRNA) has emerged as one of the most powerful therapeutic tools in recent years. It works by instructing cells to produce specific proteins, which can help repair tissues, fight disease, or replace defective genes. The success of mRNA vaccines, such as those developed by Pfizer-BioNTech and Moderna for COVID-19, demonstrated that the technology can be safe, scalable, and effective.
However, delivering mRNA into specific organs is not straightforward. It requires a protective transport system—this is where lipid nanoparticles come in. These are tiny, spherical particles made of fats that encapsulate and protect mRNA, ensuring it reaches the target cells intact. But even with this technology, targeting the heart has been especially tricky.
Why Heart Delivery Is So Difficult
Inside the body, cells have a built-in sorting mechanism called the endosome. When foreign particles like nanoparticles enter a cell, they get trapped in these tiny membrane-bound compartments. If the mRNA stays inside the endosome for too long, it begins to degrade and never reaches the cell’s cytoplasm, where it’s supposed to act. This step, called endosomal escape, is one of the biggest barriers to effective mRNA delivery.
Additionally, heart tissue is denser and less permeable than other organs, making it difficult for particles to diffuse evenly. Many nanoparticles that work in the liver or lungs fail completely in the heart.
The “Heart-on-a-Chip” Breakthrough
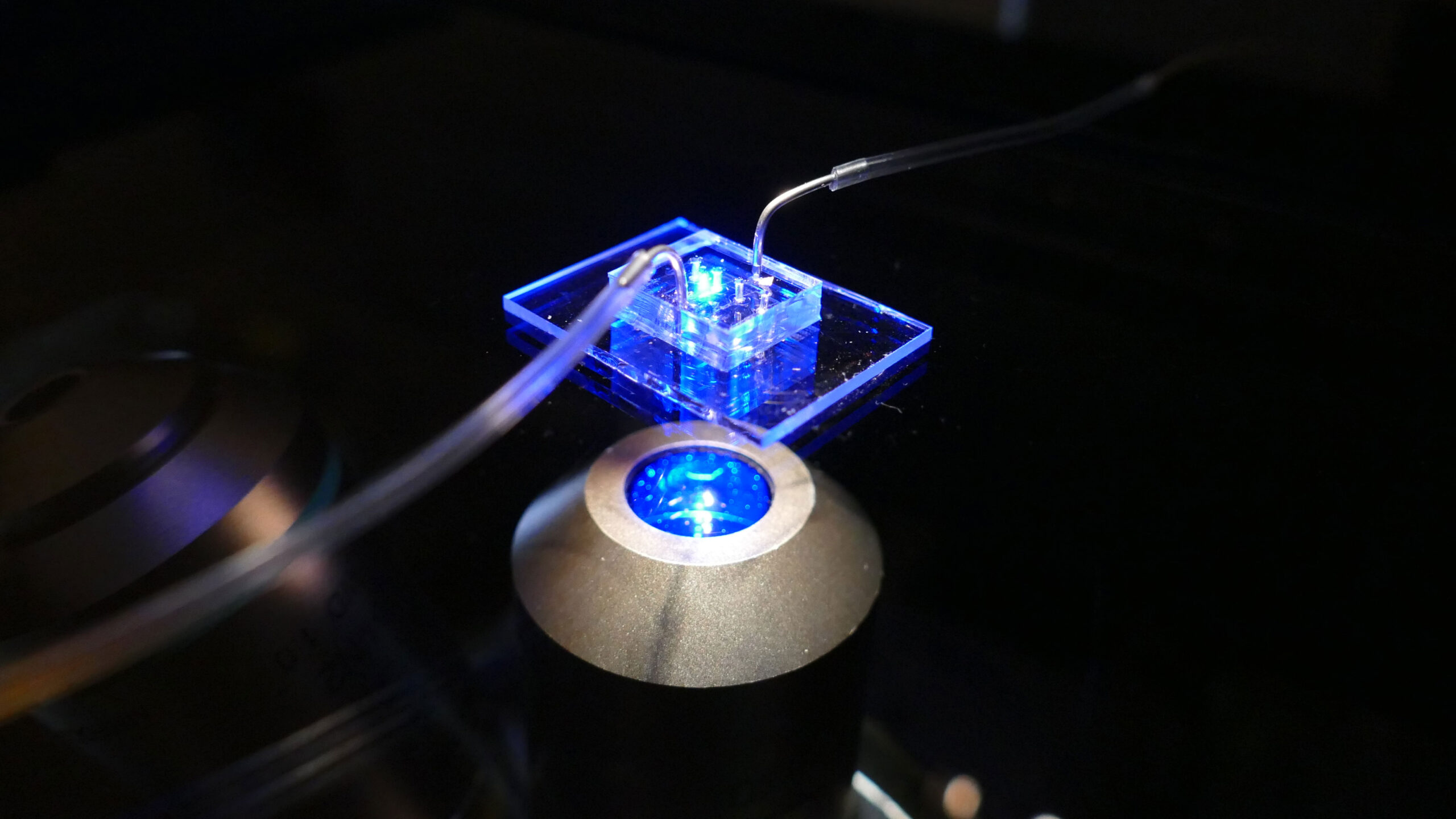
To solve this, the UC Berkeley-led team used an innovative tool known as a cardiac microphysiological system (MPS), often called a heart-on-a-chip. This is a miniaturized model of a human heart built using living human cells inside a microfluidic device—essentially a chip with channels thinner than a human hair.
Within these channels, the researchers grew three-dimensional micromuscles, small clusters of beating heart tissue that mimic the mechanical and biological environment of the human heart. The MPS allowed them to precisely control fluid flow, oxygen levels, and nutrient delivery, creating a far more realistic testing environment than traditional flat cell cultures.
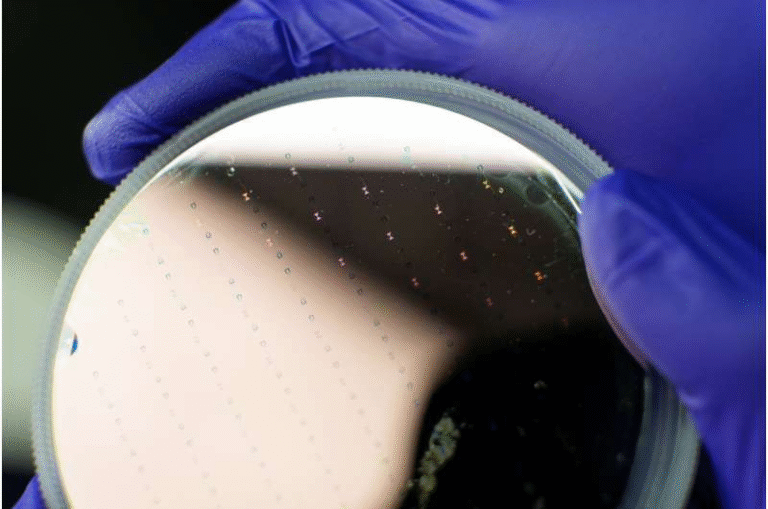
Using this advanced setup, the researchers screened various lipid nanoparticle formulations to find one capable of efficiently delivering mRNA through the dense cardiac tissue.
A New Kind of Lipid Nanoparticle
The team discovered that nanoparticles coated with a novel acid-degradable polyethylene glycol (PEG) layer performed exceptionally well. This special coating allows the nanoparticles to move more easily through the heart’s tissue and escape from endosomes once inside the cells.
The acid-sensitive PEG layer degrades in slightly acidic environments (like those inside endosomes), freeing the nanoparticle’s core and helping it release its mRNA cargo directly into the cell’s cytoplasm. This clever chemistry improves both diffusion through the heart and endosomal escape efficiency—two problems that have long held back cardiac gene therapy.
Testing the Nanoparticles in Mice
After identifying the most effective LNP formulation in their heart-on-a-chip model, the researchers moved on to in vivo testing. They injected the same nanoparticles into mouse hearts and observed how well they delivered mRNA.
The results mirrored their in vitro findings: the acid-degradable PEG-LNPs successfully delivered mRNA to cardiomyocytes and produced strong gene expression. Importantly, the new nanoparticles caused less off-target accumulation in the liver, a common issue in nanoparticle-based therapies. This finding suggests that the model used for screening—combining MPS with LNP formulation testing—accurately predicts how the particles will behave in living systems.
What Makes This Study Special
According to the research team, the success of their organ-on-a-chip approach could significantly accelerate the development of heart-targeted therapies. By using human cell-based microtissues instead of animal models for early testing, scientists can obtain faster and more reliable predictions about which nanoparticle designs will work in humans.
This shift could reduce the need for early-stage animal testing, lower research costs, and shorten the time from laboratory discovery to clinical trials. It also paves the way for designing personalized LNP formulations that match specific patient needs or genetic conditions.
Potential Applications of Heart-Targeted mRNA
The implications of this work go beyond just one experiment. If heart-targeted LNPs become reliable, they could be used in several promising ways:
- Heart failure treatments that restore or replace damaged proteins in cardiomyocytes.
- Gene correction therapies for inherited heart disorders such as hypertrophic cardiomyopathy.
- Cardioprotective treatments that prevent damage after a heart attack by delivering protective factors directly to heart tissue.
- Regenerative medicine, where mRNA could encourage new heart tissue growth.
These possibilities, once purely theoretical, are becoming more realistic thanks to advances in materials science, cellular engineering, and microphysiological modeling.
Broader Significance of Organs-on-Chips
The heart-on-a-chip is part of a larger scientific movement toward organ-on-a-chip systems—miniaturized, lab-grown models of organs like the heart, liver, lung, and brain. These platforms combine human stem cells with microengineering to recreate the physical and biological environment of real tissues.
By mimicking human physiology more accurately than animal models, these chips help scientists test drugs, study diseases, and screen new therapies with greater precision. For pharmaceutical companies, organ-on-chip systems could cut development costs and reduce the failure rates that plague traditional preclinical testing.
In the context of mRNA therapeutics, these chips could dramatically speed up the discovery of safe, targeted delivery methods for different organs, not just the heart.
The Road Ahead
Despite the promise, several challenges remain before this technology reaches human clinical trials. Translating results from mice to humans involves addressing differences in immune responses, blood circulation, and nanoparticle metabolism. Researchers also need to ensure that the LNPs do not trigger inflammation or cause unintended effects in other organs.
Long-term safety and stability are other key factors. For gene therapies to work effectively, the mRNA must remain active long enough to produce therapeutic effects but not so long that it causes toxicity.
Nevertheless, this discovery provides a clear proof of concept: it is possible to design LNPs that target and deliver mRNA directly to heart muscle cells. If refined and scaled up, this could revolutionize how we treat heart failure and other cardiac conditions.