How Light Suppresses Virulence in an Antibiotic-Resistant Pathogen
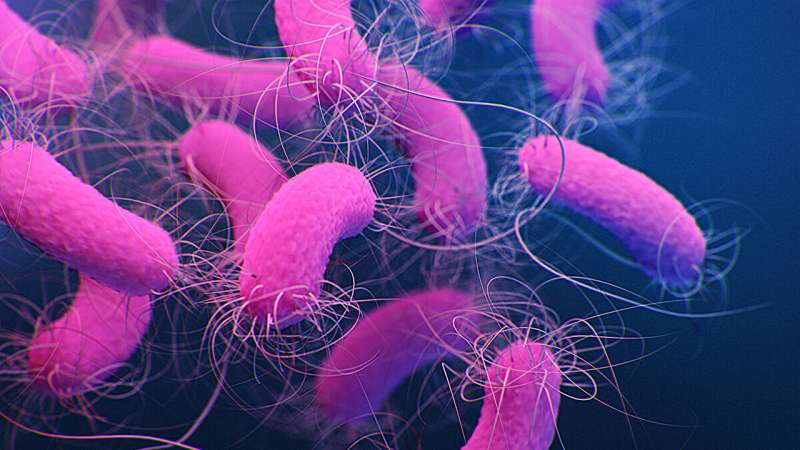
Light is one of the most universal environmental signals on Earth. From regulating human sleep cycles to guiding plant growth, its influence spans all forms of life. What is becoming increasingly clear is that light also plays a surprisingly important role in shaping the behavior of bacteria, including some of the most dangerous human pathogens. A recent study has revealed how specific wavelengths of light can suppress virulence and biofilm formation in Pseudomonas aeruginosa, a notorious antibiotic-resistant bacterium responsible for severe hospital-acquired infections.
Why Pseudomonas aeruginosa Is Such a Serious Threat
Pseudomonas aeruginosa is commonly found in soil and water, but in clinical settings it becomes a major problem. It frequently infects patients with weakened immune systems, those suffering from lung diseases such as cystic fibrosis, and individuals with large wounds or burns. One of the reasons it is so difficult to treat is its ability to form biofilms.
Biofilms are tightly packed bacterial communities that stick to surfaces like medical implants, catheters, or lung tissue. Once bacteria are embedded in a biofilm, they become far more resistant to antibiotics and immune system attacks. This makes infections persistent, chronic, and sometimes life-threatening. Understanding how to prevent or disrupt biofilm formation has therefore become a critical goal in modern microbiology.
The Discovery That Light Changes Bacterial Behavior
In 2019, researchers led by Sampriti Mukherjee at the University of Chicago made a striking observation: exposure to far-red light, a wavelength near the infrared part of the spectrum, prevented Pseudomonas aeruginosa from forming biofilms. Importantly, this type of light does not kill the bacteria. Instead, it acts as a signal, telling the pathogen to alter its behavior.
Building on that initial discovery, Mukherjee’s team wanted to understand exactly how the bacterium senses light and how that signal is translated into changes in virulence. Their latest findings, published in Nature Communications, provide a detailed molecular explanation of this process.
A Newly Identified Photosensing System
Unlike plants, Pseudomonas aeruginosa does not use light for photosynthesis. Instead, it uses light as information. The new study shows that far-red light activates a previously uncharacterized photosensing cascade inside the bacterium. This cascade ultimately leads to the suppression of genes responsible for biofilm formation and virulence factor production.
At the heart of this system is a newly identified small protein called DimA. This microprotein is located in the space between the inner and outer membranes of the bacterial cell. When far-red light is present, DimA becomes active and triggers a chain of molecular events that reshape the bacterium’s behavior.
How the Researchers Uncovered the Mechanism
To track how light affects gene expression, the research team used a luciferase reporter system. Luciferase is a protein that produces light, and by attaching its gene to promoters that control virulence genes, the scientists could easily see when those genes were turned on or off.
When Pseudomonas aeruginosa was exposed to far-red light, the luciferase reporter remained silent. This showed that the virulence genes were not being expressed. In contrast, when the researchers genetically disrupted the photosensing pathway, the bacteria produced higher levels of virulence factors, confirming that the light-sensing system actively suppresses pathogenic behavior.
During these experiments, Dimitrios Manias, the study’s lead author, identified the previously unknown gene that encodes DimA. Further analysis revealed that DimA initiates a process known as regulated intramembrane proteolysis, a controlled protein-cutting mechanism that activates transcription factors responsible for shutting down biofilm and virulence genes.
Why DimA Is Such an Important Finding
DimA acts as a positive regulator of the light-sensing pathway. This means it does not merely participate in the process but actively drives it forward. The discovery of this protein opens up new possibilities for intervention. If scientists can find ways to artificially increase DimA activity or mimic its effects, it may be possible to prevent biofilm formation even without relying on antibiotics.
This is especially significant in an era of rising antibiotic resistance, where traditional drugs are losing their effectiveness.
Light as a Non-Toxic Control Signal
During the COVID-19 pandemic, many people became familiar with the use of UV or blue light to kill microbes on surfaces. Far-red light works very differently. It does not damage bacterial DNA or membranes. Instead, it provides environmental information that bacteria interpret to adjust their behavior.
In other words, far-red light does not act as a weapon but as a switch, turning down the pathogen’s ability to cause harm.
A System Shared Across Other Bacteria
One of the most intriguing aspects of this discovery is that the same photosensing system appears in other Pseudomonas species. This suggests that light sensing may play broader roles beyond infection, possibly influencing how bacteria behave in natural environments.
For example, bacteria living in soil around plant roots may use light intensity to sense how deep they are buried. In contrast, bacteria inside the human body, such as in the lungs, experience near-total darkness, which could promote virulence and biofilm formation.
Environmental Light and Bacterial Decision-Making
The researchers propose that this photosensing cascade functions like an hourglass. Light exposure starts the process, but the response does not shut off instantly when the light disappears. Instead, the system gradually winds down, allowing bacteria to respond smoothly to changing environmental conditions such as cloud cover or shifting soil layers.
This nuanced response suggests that bacteria have evolved sophisticated ways to integrate environmental signals over time, rather than reacting in an all-or-nothing fashion.
What This Means for Future Medical Applications
Understanding how light suppresses virulence in Pseudomonas aeruginosa could lead to entirely new treatment strategies. Rather than trying to kill bacteria outright, future therapies might focus on disarming pathogens, making them less capable of causing disease.
Such approaches could reduce selective pressure for antibiotic resistance and complement existing treatments. While practical medical applications are still a long way off, the discovery of DimA and its role in light sensing represents a major step forward.
A Growing Field of Research
Photosensing in non-photosynthetic bacteria remains a largely unexplored area of microbiology. This study highlights how much remains to be learned about the hidden ways bacteria interact with their environment. As researchers continue to uncover these mechanisms, light may emerge as a powerful and subtle tool for controlling bacterial behavior.
Research Paper:
https://www.nature.com/articles/s41467-025-66862-x