How Polymyxin Antibiotics Break Bacteria’s Armor – And Why Dormant Cells Survive

Scientists from University College London (UCL) and Imperial College London have uncovered exactly how a powerful class of antibiotics, called polymyxins, destroy the protective shield of some of the world’s most dangerous bacteria. The findings, published in Nature Microbiology on September 29, 2025, explain a long-standing mystery — how these “last-resort” antibiotics breach the armor of Gram-negative bacteria, and why they fail against dormant, sleeping bacterial cells.
This new research not only shows how polymyxins work, but also reveals why they sometimes don’t — offering new clues on how to make them more effective against persistent infections that keep coming back.
What Are Polymyxins?
Polymyxins are a family of antibiotics first discovered over 80 years ago. Among them, Polymyxin B and Polymyxin E (colistin) are still used today, but only as a last defense when other antibiotics fail. They are especially useful against Gram-negative bacteria like E. coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa — microbes responsible for many drug-resistant hospital infections.
Gram-negative bacteria have a unique two-layered cell envelope. The outer layer, called the outer membrane, is made mostly of a molecule known as lipopolysaccharide (LPS). This LPS layer acts like armor, blocking many antibiotics from entering the cell. Beneath it lies the inner membrane, which encloses the cell’s vital contents.
Scientists have long known that polymyxins can damage these membranes, but exactly how they manage to do it — and why some bacteria survive the attack — remained a puzzle until now.
Watching Bacteria’s Armor Collapse in Real Time
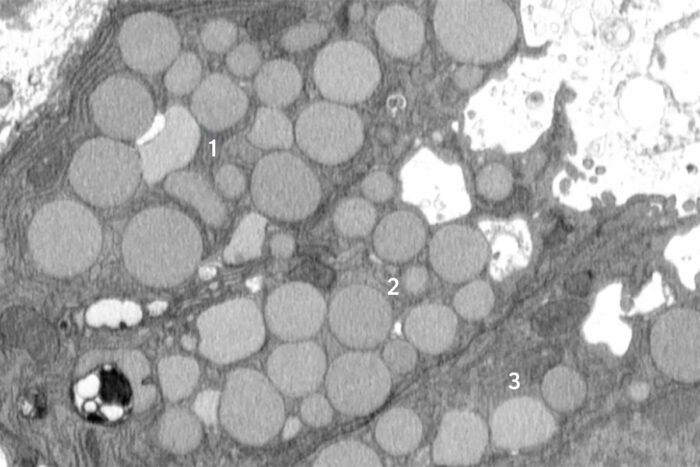
To solve the mystery, the research team used a combination of advanced imaging and biochemical experiments to actually watch what happens to bacteria under attack by polymyxins.
At the London Centre for Nanotechnology at UCL, they used a technique called atomic force microscopy (AFM). It involves a tiny needle — only a few nanometers wide — that “feels” the surface of living bacterial cells, creating detailed 3D images of their outer structure.
When E. coli cells were exposed to Polymyxin B, the researchers saw the surface start to bulge and form bumps within minutes. Over time, these cells began shedding pieces of their outer membrane, as if their armor was breaking apart from the inside.
The images revealed something remarkable: the antibiotic wasn’t just tearing through the membrane by brute force — it was making the bacteria destroy their own armor.
The Overproduction and Shedding Mechanism
The key discovery was that Polymyxin B drives bacteria to overproduce and shed their protective layer. Under normal conditions, bacteria continuously make small amounts of LPS to maintain their outer membrane. But when polymyxin B binds to that layer, it seems to trigger a panic response — the bacteria start making more LPS and pushing it out at an unsustainable rate.
This overproduction and shedding process eventually creates holes and weak spots in the outer membrane. These gaps allow the antibiotic to penetrate deeper, reaching the inner membrane where it can disrupt essential functions and kill the cell.
In other words, polymyxins trick the bacteria into overworking themselves until their armor falls apart.
When Bacteria Go to Sleep, the Antibiotic Fails
But here’s the twist that changes everything: this process only works when the bacteria are active and metabolically awake.
If the bacteria are dormant — in a resting or “hibernation-like” state — they don’t make or repair their outer membrane. That means polymyxin B has nothing to interfere with, and the antibiotic can’t break through.
In their experiments, the researchers found that when E. coli cells were active and growing, Polymyxin B killed them efficiently. But when the same bacteria were inactive, the drug did almost nothing.
Dormancy is a clever bacterial survival strategy. When conditions are bad — such as low nutrients or antibiotic exposure — some bacteria slow down their metabolism and “go to sleep.” They can stay in this state for years, waiting until the environment becomes favorable again. When they “wake up,” they resume growth, often causing relapsing or chronic infections that are difficult to treat.
This new study shows that polymyxins are powerless against these sleeping bacteria, explaining why some infections return even after strong antibiotic treatment.
Sugar Wakes Up Bacteria — and Makes the Antibiotic Work Again
To test the theory, the scientists ran an intriguing experiment. They added sugar (a food source) to the dormant E. coli cells, allowing them to wake up and start metabolizing again. Once that happened, Polymyxin B became effective — but only after a short delay of about 15 minutes, which is how long it took for the cells to reactivate and resume producing their outer membrane.
In these “woken-up” cells, the antibiotic once again caused visible bulges and armor shedding. Without the sugar, the antibiotic bound to the cell surface but didn’t cause any significant damage.
This clearly showed that the lethal action of polymyxin B depends on the bacteria being metabolically active.
A Two-Step Killing Process
The researchers describe polymyxin’s killing process as two distinct steps:
- Energy-dependent outer membrane disruption – The antibiotic binds to LPS and triggers the bacteria to overproduce and shed it. This stage needs energy, which means it only happens when the bacteria are active.
- Energy-independent inner membrane permeabilization – Once holes appear in the outer layer, polymyxin B reaches the inner membrane, where it disrupts it and kills the cell.
The first step is where the antibiotic either succeeds or fails. Without energy, the bacteria never reach the vulnerable stage.
Why Some Bacteria Are Resistant
The study also looked at bacteria carrying the mcr-1 resistance gene, which has been spreading worldwide since its discovery in 2015. This gene modifies the LPS molecules in the outer membrane, preventing polymyxin B from binding properly.
The researchers found that in mcr-1-positive bacteria, the overproduction and shedding of LPS didn’t happen. The membrane stayed mostly intact, meaning the antibiotic couldn’t get through.
This finding supports the idea that mcr-1 blocks polymyxin’s action at the very first step — the outer membrane disruption — instead of simply reducing the antibiotic’s binding affinity.
Implications for Future Treatments
Understanding how polymyxins really work — and why they fail — could open new paths for designing more effective antibiotic treatments.
One potential strategy would be to combine polymyxins with compounds that wake up dormant bacteria or boost their metabolism just enough for the antibiotic to act. Another idea is to pair polymyxins with agents that weaken the bacterial outer membrane, so they don’t rely on the bacteria’s own activity to get inside.
Researchers also stress that doctors and scientists must consider the metabolic state of bacteria when testing antibiotics in the lab. Traditional tests usually measure how well a drug kills actively growing bacteria, but they don’t account for dormant ones — the very cells that often survive in patients.
This study provides a clearer framework for understanding why antibiotic resistance and tolerance are so difficult to overcome. It’s not just about mutations or resistance genes — it’s also about the bacteria’s ability to switch between active and inactive states.
The Imaging Technology Behind the Discovery
The images that made this discovery possible were captured using atomic force microscopy (AFM) — a technique capable of visualizing individual bacteria at nanoscale resolution, far beyond what standard light microscopes can achieve.
By scanning a sharp probe across the surface of living cells, researchers could actually see the physical collapse of the bacterial armor in real time.
Additional tools, like scanning electron microscopy (SEM) and fluorescence assays, confirmed what the images showed — polymyxin B causes a massive structural breakdown of the outer membrane in active bacteria but leaves dormant ones largely unharmed.
Why Polymyxins Are Still So Important
Despite being discovered in the 1940s, polymyxins remain one of the few antibiotic classes effective against the most stubborn Gram-negative “superbugs”. Unfortunately, they’re also known for being toxic to human kidneys and nerves, which limits how much can safely be used in treatment.
That’s why scientists are eager to find ways to improve their precision and reduce their side effects. Knowing exactly how polymyxins interact with bacterial membranes is a big step toward designing safer, more effective derivatives or combination therapies.
The Bigger Picture: Antibiotic Resistance and Dormancy
Antibiotic resistance continues to be a global crisis. Each year, over a million people die from drug-resistant infections, and the number is expected to rise sharply in the coming decades.
One of the hardest challenges is dealing with tolerant or dormant bacteria. These cells aren’t technically resistant — the antibiotics still work against them in theory — but since they “shut down” when attacked, the drugs can’t reach their targets. Once the antibiotic is gone, they wake up and multiply again.
This new research gives a clear mechanistic explanation for why that happens in the case of polymyxins. More broadly, it highlights that bacterial metabolism plays a central role in how antibiotics succeed or fail.
Funding and Collaboration
The work was supported by the Biotechnology and Biological Sciences Research Council (BBSRC), the Engineering and Physical Sciences Research Council (EPSRC) — both part of UK Research and Innovation — and by Wellcome.
Researchers involved came from UCL, Imperial College London, and the University of Nottingham, including Carolina Borrelli, Edward Douglas, Sophia Riley, Aikaterini Lemonidi, Gerald Larrouy-Maumus, Wen-Jung Lu, Boyan Bonev, Andrew Edwards, and Bart Hoogenboom.
Conclusion
This discovery finally clarifies what’s happening when polymyxin antibiotics attack bacteria — and why they sometimes fail. It also provides a path forward: by understanding how bacterial energy and metabolism affect antibiotic action, researchers can begin designing smarter ways to outsmart these pathogens.
The battle against antibiotic-resistant infections is far from over, but breakthroughs like this one bring us a step closer to truly effective, lasting solutions.
Research Reference:
Polymyxin B lethality requires energy-dependent outer membrane disruption – Nature Microbiology (2025)