How Your Daily Coffee Could Be Weakening Antibiotics

Most of us can’t imagine starting the day without a cup of coffee, but new research suggests our beloved caffeine fix might be doing more than just keeping us awake.
A team of scientists from the Universities of Tübingen and Würzburg has found that common dietary ingredients, including caffeine, may influence how bacteria respond to antibiotics. And that could have real implications for the way we treat infections.
Everyday Ingredients With Surprising Effects
We tend to think of antibiotics as powerful, precise medicines that work independently of what else we eat or drink. But this new study flips that idea on its head. Researchers discovered that substances in our daily diets—things as ordinary as caffeine—can alter bacterial defenses, making certain antibiotics less effective.
To test this, the team examined 94 different compounds, ranging from antibiotics and prescription drugs to food-related substances. They wanted to see how these compounds affected Escherichia coli (E. coli), a bacterium known for causing various infections. What they uncovered was that bacteria are not passive targets. Instead, they constantly monitor their environment and adjust their internal systems in response to outside signals.
How Bacteria Outsmart Drugs
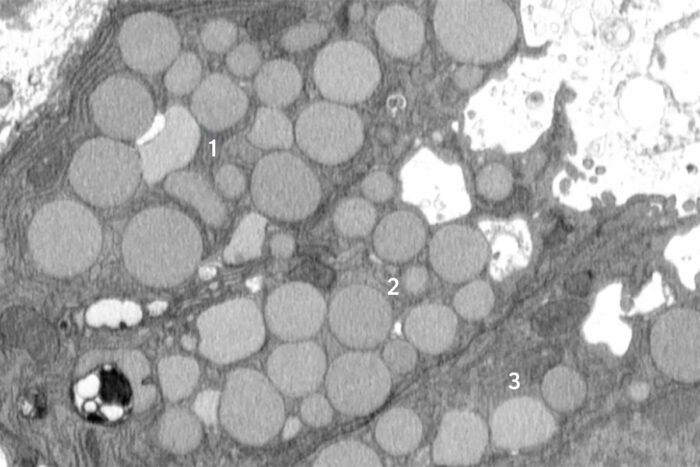
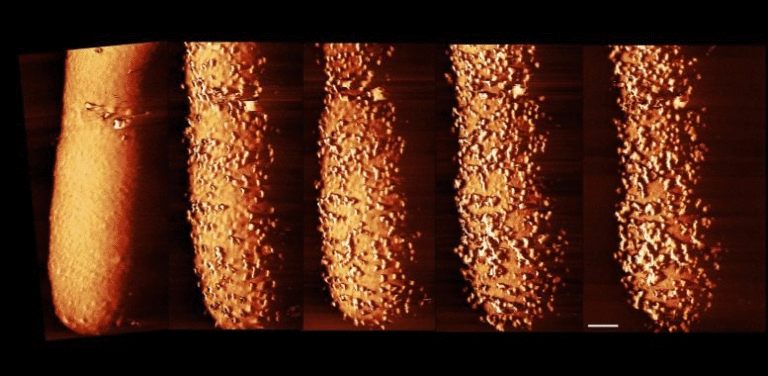
The key players here are transport proteins, which act like gates and pumps in the bacterial membrane. They control what enters and exits the bacterial cell. Antibiotics rely on these systems to reach their targets inside the cell. But the research showed that caffeine, and potentially other dietary substances, can disrupt this delicate balance.
Caffeine sets off a chain reaction inside E. coli. It activates certain gene regulators, particularly one called Rob, which then alters several transport proteins. The end result? Reduced uptake of antibiotics such as ciprofloxacin. Simply put, caffeine makes it harder for the drug to get inside the bacteria—dulling its effectiveness.
The researchers describe this as an “antagonistic interaction”: a situation where a common substance doesn’t directly kill bacteria, but still makes antibiotics work less effectively.
Not All Bacteria React the Same
Here’s where it gets even more interesting. While caffeine weakened antibiotics in E. coli, it didn’t have the same effect on Salmonella enterica, a closely related bacterium. This shows that even similar bacterial species can respond differently to the exact same environmental cues. It all depends on their internal transport systems and how they’re wired to react.
This difference highlights why tackling antibiotic resistance is so complex. It’s not just about genes that make bacteria resistant. Sometimes, the environment—including what we eat and drink—can shift bacterial behavior in subtle but meaningful ways.
Why This Matters
The study sheds light on what researchers call “low-level” antibiotic resistance. Unlike the classic form of resistance, which is driven by genetic mutations or resistance genes, this type comes from everyday environmental adjustments inside bacteria.
This has real-world consequences. If certain foods or drinks can reduce antibiotic effectiveness, doctors might need to rethink treatment strategies. For example, patients may one day receive guidance not just on how much of a drug to take, but also on what substances to avoid while on medication.
As one of the researchers noted, this is a reminder of how science helps us connect the dots between everyday habits and global health challenges. Something as routine as sipping a coffee could be nudging bacteria to resist life-saving drugs—without us even realizing it.
Looking Ahead
The findings, published in PLOS Biology, open the door for future studies into how diet and medicine interact in unexpected ways. It raises questions like: Should certain dietary guidelines accompany antibiotic prescriptions? Could other common ingredients—tea, chocolate, or even prescription drugs—be playing similar roles?
For now, this doesn’t mean you need to ditch your morning latte when you’re prescribed antibiotics. But it does mean scientists are paying closer attention to the hidden interactions between our lifestyles and the microscopic world inside us.
And who knows? In the future, your doctor’s advice may include not just “take with water,” but also “skip the coffee for now.”
Source: “Systematic screen uncovers regulator contributions to chemical cues in Escherichia coli” by Christoph Binsfeld, Roberto Olayo-Alarcon, Lucía Pérez Jiménez, Morgane Wartel, Mara Stadler, André Mateus, Christian Müller and Ana Rita Brochado, 22 July 2025, PLOS Biology.
DOI: 10.1371/journal.pbio.3003260