New Study Reveals How Neutrophils Trigger Early Atopic Dermatitis Flares in Dogs

A new scientific study from North Carolina State University has shed light on a part of the immune system that has largely flown under the radar in atopic dermatitis research: neutrophils. These white blood cells, best known for their role in fighting infections, appear to play an important role in the very early stages of allergic skin flare-ups in dogs. The findings not only advance veterinary science but could also have meaningful implications for human atopic dermatitis, a condition that affects millions worldwide.
The study, published in the peer-reviewed journal Frontiers in Allergy, focuses on understanding how neutrophils behave during the initial phases of canine atopic dermatitis (AD)—a chronic, inflammatory skin disease commonly associated with allergies.
Understanding Atopic Dermatitis in Dogs
Atopic dermatitis is a type of eczema characterized by itchy, inflamed, and irritated skin. In dogs, it is often triggered by environmental allergens such as house dust mites, pollen, or mold. The condition is chronic, meaning it tends to flare up repeatedly over time rather than resolving completely.
While AD has been extensively studied, most research has focused on immune cells such as T cells, mast cells, eosinophils, and cytokines. Neutrophils, despite being one of the most abundant white blood cells in circulation, had not been thoroughly examined in the context of allergic skin disease—especially in dogs.
This research set out to address that gap.
Why Neutrophils Matter
Neutrophils are part of the body’s innate immune system, meaning they are among the first responders when the body encounters a perceived threat. Their primary function is to identify, engulf, and destroy foreign invaders, such as bacteria or allergens. They also release chemical signals that can recruit other immune cells to the site of inflammation.
Until recently, neutrophils were not considered central players in atopic dermatitis. However, earlier research using mouse models hinted at a possible connection. The NC State research team decided to explore whether this connection also exists in a canine model, which more closely mirrors human disease in terms of environment and immune responses.
How the Study Was Conducted
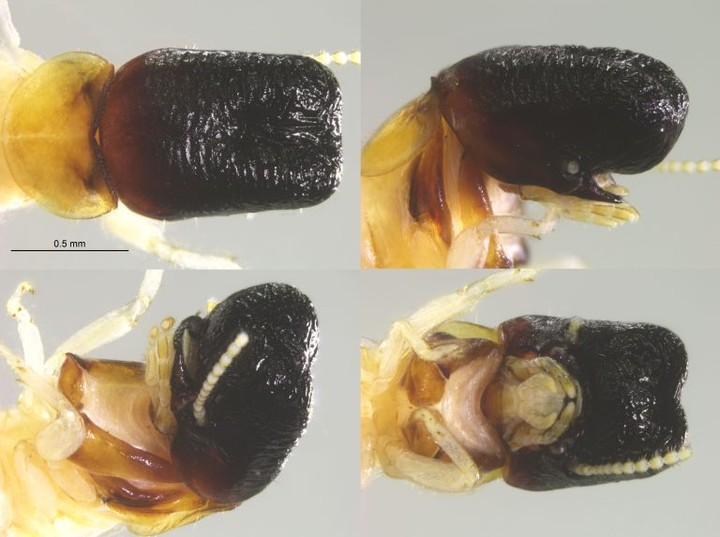
The researchers examined skin samples from nine dogs in total. Four dogs had house dust mite–induced atopic dermatitis, while five dogs served as healthy controls.
To trigger allergic responses, the dogs with AD were exposed to house dust mites, a well-known allergen in both dogs and humans. Skin biopsies were then collected at three specific time points following allergen exposure:
- 24 hours
- 48 hours
- 96 hours
The samples were analyzed using immunofluorescent staining, a laboratory technique that allows scientists to identify and measure specific immune cells within tissue. This approach made it possible to track the presence and activity of neutrophils over time.
Key Findings of the Research
The results revealed a clear and time-dependent pattern of neutrophil activity during allergic skin flare-ups:
- Neutrophils were detected early, within 24 hours of allergen exposure.
- Their numbers peaked around 48 hours, marking the height of their involvement.
- By 96 hours, neutrophil levels had significantly declined, suggesting their role is limited to the early phase of the flare.
This pattern indicates that neutrophils are not random bystanders but are actively involved at the onset of inflammation. Their presence during this narrow window suggests they may help shape how the rest of the immune response unfolds.
What remains unclear—and is a focus for future research—is what exactly neutrophils are doing during this phase. They may be clearing allergens, recruiting other immune cells, amplifying inflammation, or possibly doing all of these things simultaneously.
Why the 48-Hour Mark Is Important
The study highlights 48 hours after allergen exposure as a critical point in the immune response. This is when neutrophil activity is at its highest, suggesting that interventions targeting neutrophils during this window could potentially reduce the severity or duration of flare-ups.
Understanding this timing is especially important for developing new therapeutic strategies, as most current treatments focus on suppressing inflammation after it is already well established.
Broader Implications for Treatment
This research opens up a new pathway for studying atopic dermatitis. By identifying neutrophils as early contributors, scientists now have an additional immune mechanism to investigate when developing treatments.
From a veterinary perspective, this could eventually lead to more targeted therapies for dogs, potentially improving quality of life for pets that suffer from chronic itching and skin damage.
From a human health standpoint, the findings are equally compelling.
Why Dogs Are Important Models for Human Disease
Dogs share our living spaces, environmental exposures, and many disease processes. Unlike laboratory mice, they develop allergic conditions naturally, making them valuable models for studying complex diseases like atopic dermatitis.
Because canine and human AD share many similarities, insights gained from dogs often translate more effectively to human medicine. A better understanding of neutrophil behavior in dogs may therefore help researchers identify new therapeutic targets for people with eczema and related conditions.
The Researchers Behind the Study
The study was led by Santosh Mishra, an associate professor of molecular biomedical sciences at NC State, who served as the corresponding author. The first author is Chie Tamamoto-Mochizuki, a former NC State postdoctoral researcher who is now affiliated with the University of Tennessee, Knoxville.
Their work represents an important early step rather than a final answer. The researchers emphasize that skin is a highly complex organ, and allergic inflammation involves many overlapping immune pathways.
What Comes Next
Future studies will aim to track neutrophil activity throughout the entire course of a flare-up, not just the early stages. Researchers are also interested in understanding how neutrophils interact with other immune cells and whether modifying their behavior could alter disease progression.
As research continues, neutrophils may move from being overlooked players to key targets in managing allergic skin disease.
Extra Context: Neutrophils and Allergic Disease
Beyond atopic dermatitis, neutrophils are increasingly being studied in other inflammatory and allergic conditions, including asthma and psoriasis. They are known to release enzymes, reactive oxygen species, and signaling molecules that can significantly influence tissue inflammation.
This growing body of research suggests that neutrophils are far more versatile—and influential—than previously thought.
Research Reference
Investigation of neutrophil infiltration in the acute canine atopic dermatitis model
https://www.frontiersin.org/articles/10.3389/falgy.2025.1716716/full