Scientists Develop a Way to Protect T Cells From Cancer-Induced Exhaustion
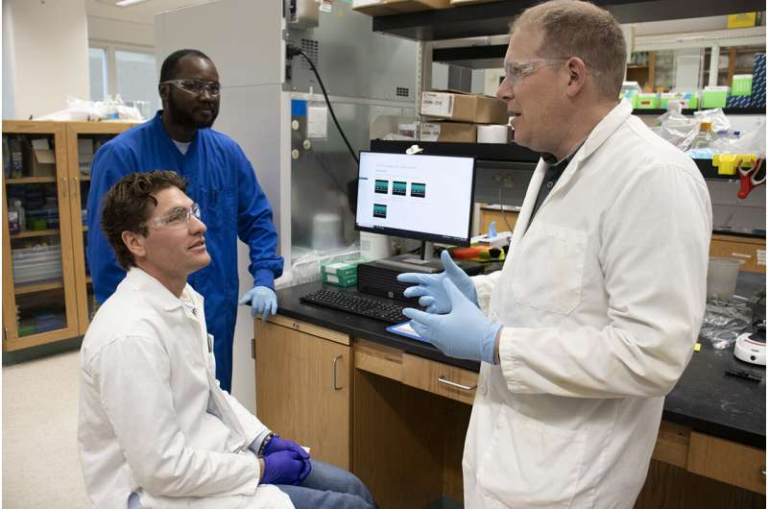
Researchers at the University of Pittsburgh have uncovered an important new insight into how cancer weakens the immune system’s most effective fighters, the T cells, and have developed a potential way to make these cells resistant to tumor-induced damage.
Their work, published in the journal Immunity in September 2025, shows that the toxic environment inside tumors directly harms telomeres in T cells, pushing them into a dysfunctional and exhausted state. By designing a targeted antioxidant approach, the team managed to restore T cell function in mice, opening a pathway to improving cancer immunotherapy.
Tumor Environments and Their Effect on T Cells
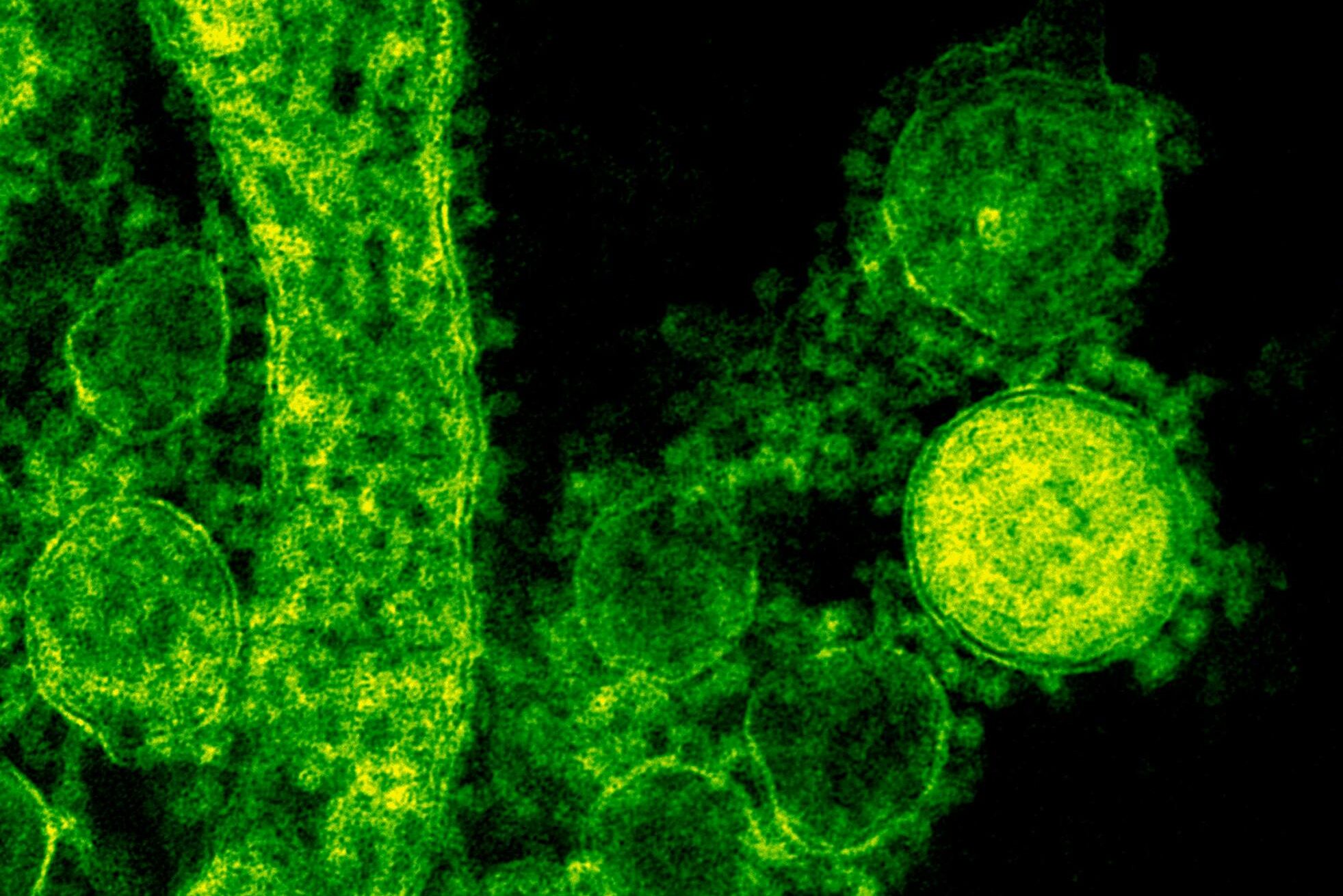
Tumors are not just clusters of uncontrolled cells. They create their own hostile microenvironments. Inside a tumor, oxygen levels are low (hypoxia), acidity is high, and nutrients are scarce. All of this puts extreme pressure on immune cells, especially T cells, which are responsible for directly attacking cancer.
When T cells are placed in these environments, their mitochondria (the cell’s energy-producing engines) become stressed and overloaded. Under stress, mitochondria produce excessive reactive oxygen species (ROS)—highly reactive molecules that can damage DNA and proteins. The Pittsburgh team discovered that these ROS migrate to the cell nucleus and specifically harm telomeres, which are the protective caps on the ends of chromosomes.

This telomere damage drives T cells into a state called exhaustion, where they lose the ability to divide effectively or destroy cancer cells. Exhausted T cells are a major roadblock in immunotherapy, making this finding particularly significant.
The Unexpected Connection Between Mitochondria and Telomeres
The researchers, led by Dayana Rivadeneira and Greg Delgoffe, did not originally set out to study telomeres. Their initial focus was on how mitochondrial stress undermines T cell performance. But when they collaborated with Patricia Opresko, an expert in telomere biology, and the late Marcel Bruchez from Carnegie Mellon University, they uncovered a surprising link between mitochondria and telomere damage.
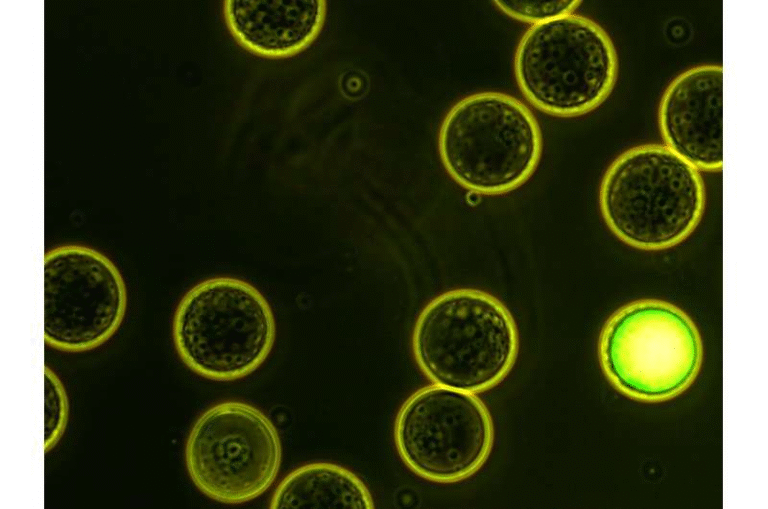
To test this, they engineered mice with a chemo-optogenetic system. In this system, exposing cells to far-red light could trigger oxidative stress either directly in mitochondria or directly at telomeres.
The results were striking. When oxidative damage was induced in either location, the outcome was the same: T cells became dysfunctional. This showed a two-way communication between mitochondria and telomeres. Damaging mitochondria caused telomere damage, and damaging telomeres fed signals back to mitochondria that also led to dysfunction. This crosstalk suggests that both parts of the cell are deeply interconnected in regulating immune function.
Testing Antioxidants to Rescue T Cells
Since ROS were identified as the culprit behind telomere instability, the team hypothesized that antioxidants could prevent this damage. Instead of flooding the cells with general antioxidants, they created a telomere-specific antioxidant strategy.
The researchers engineered mouse T cells so that an antioxidant enzyme was tethered directly to telomeres through a telomere-binding protein. This ensured that the antioxidant neutralized ROS exactly where damage occurred, at the chromosome ends.
When these modified T cells were transferred into mice with aggressive melanoma tumors, the results were highly promising. The mice that received telomere-protected T cells had smaller tumors and significantly improved survival rates compared to those that received unmodified T cells.
This experiment strongly suggests that targeted antioxidant therapy could rescue T cell function in cancer, even under the harsh conditions of the tumor environment.
Implications for CAR-T Therapy and Other Immunotherapies
One of the most exciting aspects of this research is its potential application to CAR-T cell therapy. CAR-T involves removing a patient’s T cells, genetically engineering them to recognize and attack cancer, and then reinfusing them into the body. While CAR-T has shown success in some blood cancers, it often struggles against solid tumors because T cells become exhausted in the tumor environment.
The Pittsburgh team believes that incorporating telomere-targeted antioxidants into CAR-T protocols could make the modified T cells “bulletproof” against oxidative stress. Since CAR-T already involves genetic modification, adding an extra step to tether antioxidants to telomeres would be relatively straightforward in principle.
This strategy could also apply to other adoptive cell therapies, such as those using tumor-infiltrating lymphocytes (TILs).
Next Steps Toward Human Application
So far, the research has been conducted in mouse models. The next challenge is translating the approach to human T cells. The team is actively working on developing a human-compatible telomere-specific antioxidant system. Their long-term goal is to bring this into clinical trials.
Another research direction is exploring how chemotherapy—which is widely used before or alongside immunotherapy—affects telomere health in T cells. Chemotherapy itself can cause DNA and telomere damage, and this may interfere with the ability of patients to respond to immunotherapy. If telomere-protection strategies can mitigate this effect, it could lead to better treatment outcomes.
Why Telomeres Matter in Immune Health
To better understand why this discovery is so important, it helps to know more about telomeres.
- What they are: Telomeres are repetitive DNA sequences at the ends of chromosomes. Their main job is to prevent chromosomes from fraying or sticking to each other during cell division.
- Natural shortening: Each time a cell divides, telomeres shorten slightly. When they become critically short, the cell can no longer divide and enters a state known as senescence.
- Oxidative damage: In addition to natural shortening, telomeres are especially vulnerable to oxidative stress. Unlike some other regions of DNA, telomeres lack strong repair mechanisms, making them fragile targets for ROS.
In immune cells like T cells, telomere health is crucial. T cells need to proliferate rapidly when fighting infections or cancer, and damaged telomeres limit their ability to do so.
The Role of Mitochondria in T Cell Function
Another important part of the story is the role of mitochondria in immune function.
- Energy production: Mitochondria generate ATP, the energy currency of the cell. For T cells to remain active and multiply, they need strong mitochondrial support.
- Stress signals: When mitochondria are damaged, they release ROS. While small amounts of ROS can be useful in signaling, excessive amounts are harmful.
- Immune exhaustion: Chronic mitochondrial stress in tumors doesn’t just lower energy—it actively pushes T cells into exhaustion, weakening the immune defense.
The discovery that mitochondrial stress and telomere damage are linked closes a major gap in understanding how tumors wear down the immune system.
Broader Implications Beyond Cancer
While this research is focused on cancer, its implications extend further. Telomere damage and mitochondrial dysfunction are common themes in aging, chronic infections, and inflammatory diseases. T cells in elderly individuals often show signs of exhaustion and shortened telomeres, which may partly explain why older patients respond less effectively to vaccines or infections.
Targeted antioxidant strategies might one day be used to strengthen immune function in other contexts, not just cancer.
Strengths and Limitations of the Study
Strengths:
- The chemo-optogenetic model used in mice allowed precise control of oxidative stress at specific sites, making the results very robust.
- The telomere-specific antioxidant approach is highly targeted, avoiding the drawbacks of broad antioxidant therapies.
- The study demonstrates clear translational potential because the strategy can be integrated into existing CAR-T workflows.
Limitations:
- The work has so far been performed in mice. Human immune cells and tumors are more complex.
- ROS play important roles in normal cell signaling. Over-suppressing them might disrupt other critical processes.
- Tumor environments include many other immunosuppressive factors beyond ROS, such as metabolic stress and immune checkpoint signals. Telomere protection might not solve all of these issues.
- Long-term safety of tethered antioxidant proteins will need thorough evaluation before clinical use.
Conclusion
This research adds a powerful new layer of understanding to how tumors disable the immune system. By linking mitochondrial stress to telomere damage, and showing that targeted antioxidants can preserve T cell function, the Pittsburgh team has opened up a new path for enhancing cancer immunotherapy.
If successfully translated to humans, this telomere-protection strategy could make future CAR-T and T cell therapies far more effective against solid tumors, potentially changing the way we approach cancer treatment.
Research Reference: Oxidative-stress-induced telomere instability drives T cell dysfunction in cancer, Immunity, 2025