A Massive Genetic Study Reveals Why Psychiatric Disorders So Often Overlap
A new large-scale genetics study has offered one of the clearest explanations yet for a long-standing puzzle in mental health: why so many people are diagnosed with more than one psychiatric disorder during their lifetime. Published in Nature in December 2025, the research shows that many psychiatric conditions are deeply connected at the genetic level, sharing common biological roots rather than being entirely separate illnesses.
The study was conducted by an international team from the Psychiatric Genomics Consortium’s Cross-Disorder Working Group, one of the largest collaborations in psychiatric research. It represents the most comprehensive genetic analysis of psychiatric disorders ever completed, both in scale and detail.
Why multiple psychiatric diagnoses are more common than we think
In clinical practice, having more than one psychiatric diagnosis is not unusual—it is actually the norm. Many people initially diagnosed with one condition later receive a second or even third diagnosis. Until now, this overlap has largely been explained through symptoms, lived experience, and environmental stressors.
This new research confirms that genetics plays a major role as well.
Psychiatry remains unique among medical specialties in that it lacks clear laboratory tests. Diagnoses are made based on observed symptoms and patient experiences rather than blood tests or imaging results. By mapping shared genetic risk, this study helps explain why symptom-based categories often blur together in real life.
An unprecedented dataset of more than six million people
The research team analyzed genetic data from over six million individuals. This included more than one million people diagnosed with at least one psychiatric disorder, alongside approximately five million individuals without a diagnosed psychiatric condition.
By comparing these datasets, researchers identified genetic variants that appear more frequently in people with specific disorders. This approach allows scientists to estimate how much genetic risk is shared across different conditions.
The study focused on 14 major psychiatric disorders, spanning childhood-onset, adult-onset, and substance-related conditions.
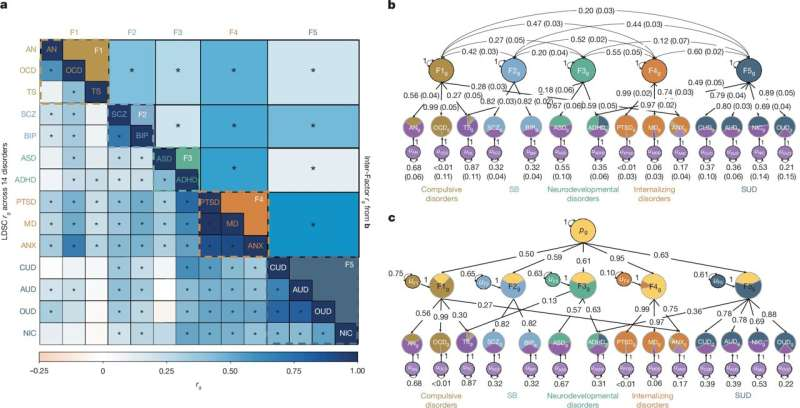
Five genetically linked families of psychiatric disorders
Using multiple advanced statistical and structural modeling techniques, the researchers discovered that these 14 disorders consistently cluster into five genetically overlapping groups. These groupings reflect shared biological pathways rather than traditional diagnostic boundaries.
1. Compulsive disorders
This group includes obsessive-compulsive disorder (OCD) and anorexia nervosa, with additional genetic overlap seen with Tourette disorder and some anxiety disorders.
2. Internalizing disorders
This category includes major depressive disorder, anxiety disorders, and post-traumatic stress disorder (PTSD). These conditions showed some of the strongest genetic overlap in the entire study.
3. Neurodevelopmental disorders
This group consists of autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD), with partial overlap involving Tourette disorder.
4. Schizophrenia and bipolar disorder
Although traditionally classified as distinct illnesses, these two conditions were found to be closely linked genetically, sharing a large proportion of inherited risk.
5. Substance use disorders
This group includes opioid use disorder, cannabis use disorder, alcohol use disorder, and nicotine dependence, all of which showed strong shared genetic foundations.
Hundreds of shared genetic variants and chromosome hot spots
The study identified 428 genetic variants associated with more than one psychiatric disorder. In addition, researchers discovered 101 regions of the genome that act as “hot spots,” meaning they contain clusters of shared risk variants across multiple conditions.
These findings reinforce the idea that psychiatric disorders are not isolated entities. Instead, they arise from interconnected genetic systems that influence brain development, emotional regulation, and behavior in overlapping ways.
Some disorders share the majority of their genetic risk
One of the most striking results involved internalizing disorders. Major depression, anxiety disorders, and PTSD were found to share about 90% of their genetic risk, making them among the most genetically similar conditions studied.
Similarly, schizophrenia and bipolar disorder were shown to share around 66% of their genetic markers, providing strong biological evidence for why these disorders often show overlapping symptoms and why diagnosis can be challenging.
What brain cells and development reveal about psychiatric risk
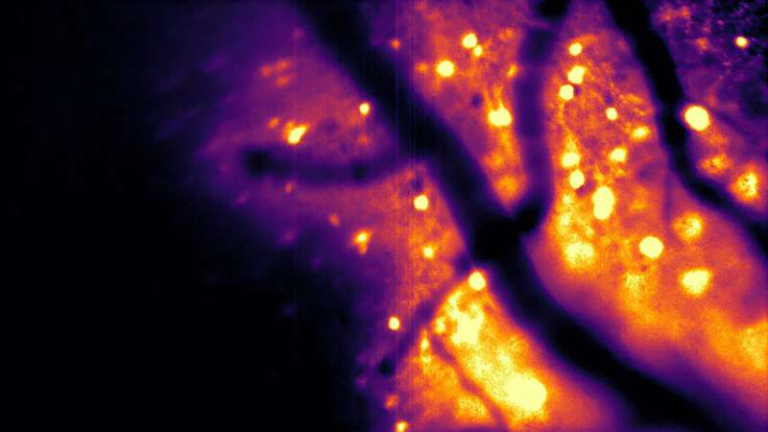
The researchers went beyond identifying shared genes and explored where and when these genes are active in the brain.
They found that disorders with high genetic overlap also share patterns of gene expression during human development and involve similar brain cell types.
For example:
- Genes linked to internalizing disorders were more commonly expressed in oligodendrocytes, cells responsible for insulating nerve fibers and supporting communication in the brain.
- Genes associated with schizophrenia and bipolar disorder were more strongly expressed in excitatory neurons, which play a key role in activating brain circuits.
These biological signatures help connect genetic findings to actual brain function, offering clues about how risk develops over time.
What this means for psychiatric diagnosis
These results provide a strong scientific foundation for rethinking how psychiatric disorders are defined. Current diagnostic systems rely heavily on symptom checklists, which can struggle to capture overlapping conditions.
The study suggests that shared biology may be just as important as distinct symptoms, and future diagnostic frameworks may benefit from incorporating genetic and neurobiological data.
This does not mean existing diagnoses are wrong—but it does highlight why strict boundaries between disorders often fail to reflect real patient experiences.
Implications for treatment and future therapies
Understanding shared genetic risk opens new possibilities for treatment. If multiple disorders arise from common biological pathways, it may be possible to:
- Repurpose existing medications for related conditions
- Develop treatments that target shared genetic mechanisms rather than individual diagnoses
- Improve early identification of people at risk for multiple disorders
This approach could be especially valuable for individuals who do not respond well to treatments designed for only one diagnosis.
Important limitations to keep in mind
While the study is groundbreaking, it does have limitations. Much of the genetic data comes from individuals of European ancestry, highlighting the need for more diverse datasets in future research.
The researchers also emphasize that genetics is only part of the picture. Environmental factors, trauma, social context, and personal experiences still play crucial roles in whether and how psychiatric disorders develop.
A step toward biologically informed psychiatry
Overall, this study marks a major step toward a more biologically grounded understanding of mental illness. By revealing how deeply connected psychiatric disorders are at the genetic level, it helps explain why comorbidity is so common—and why treating mental health conditions often requires a broad, flexible approach.
Rather than seeing psychiatric diagnoses as isolated labels, this research encourages viewing them as interconnected expressions of shared genetic vulnerability, shaped by both biology and life experience.
Research paper:
https://www.nature.com/articles/s41586-025-09820-3