A Nationwide Study Shows Brain and Nervous System Cancer Burden Varies Sharply Across the United States
A newly published nationwide study has taken a deep dive into how brain and central nervous system (CNS) cancers affect people across the United States, and the findings reveal a picture that is far from uniform. While these cancers account for only around 2% of all cancer diagnoses in the country, their impact differs significantly depending on where people live, how old they are, their sex, and their socioeconomic environment.
The research, published in JAMA Neurology, draws on data from the Global Burden of Disease (GBD) Collaborator Network, one of the most comprehensive global efforts to measure health outcomes. The study analyzes trends in CNS cancer incidence, mortality, and overall disease burden in the U.S. over a 31-year period from 1990 to 2021, offering one of the most detailed overviews of this disease category to date.
What Counts as Brain and Central Nervous System Cancer?
Brain and CNS cancers include primary tumors that originate in the brain, spinal cord, or surrounding structures. Unlike cancers that spread to the brain from other parts of the body, these tumors begin within the central nervous system itself. Although relatively rare compared to cancers like lung, breast, or colorectal cancer, CNS tumors are often more complex to treat and can lead to significant disability, even when survival improves.
Because the brain and spinal cord control essential bodily functions, even small tumors can have outsized effects on quality of life, making the broader disease burden an important metric alongside survival rates.
Key Findings From the Study
Nearly 32,000 New Cases in 2021
According to the study, almost 32,000 Americans were newly diagnosed with brain or CNS cancer in 2021. Despite advances in medical imaging, diagnostics, and treatment, the overall rate of new cases has remained largely unchanged since 1990. This stability suggests that while doctors are better at managing the disease, prevention and early risk reduction remain limited.
Fewer Deaths and Less Disability Over Time
While incidence has stayed steady, outcomes have improved modestly:
- Mortality declined by approximately 8% between 1990 and 2021
- Overall disease burden, measured in disability-adjusted life years (DALYs), fell by around 16%
DALYs combine years of life lost due to early death with years lived with disability, offering a fuller picture of how a disease affects both lifespan and daily functioning. The reduction in DALYs suggests that patients are living longer and, in some cases, managing the disease better than in previous decades.
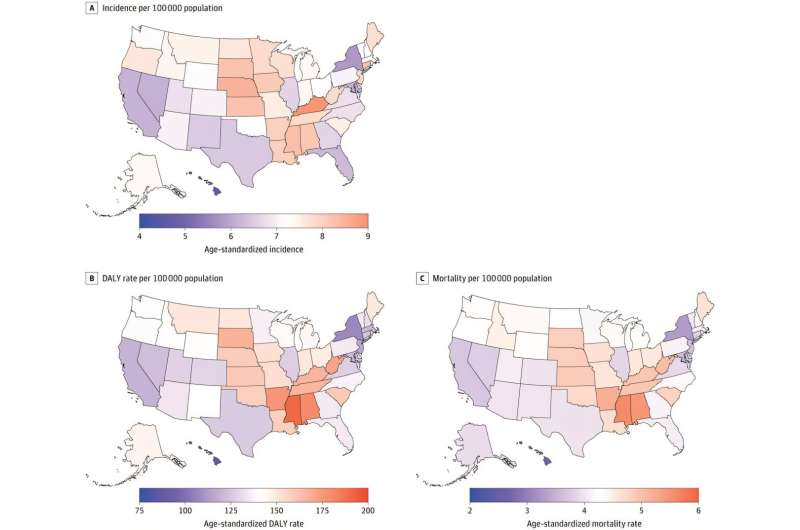
Geographic Differences Are Striking
One of the most eye-catching aspects of the study is how unevenly CNS cancer burden is distributed across the country.
States that consistently showed higher rates of illness and death include:
- Mississippi
- Alabama
- Kentucky
- Kansas
- West Virginia
These patterns have remained persistent for decades. Researchers point toward access to specialized care, regional healthcare infrastructure, socioeconomic conditions, and broader health disparities as likely contributors. States with fewer large academic medical centers or limited access to advanced neurosurgical and oncology services may face worse outcomes even when diagnosis rates are similar.
Differences by Sex and Age
Men Carry a Higher Burden
Across nearly all measures, men experienced a higher burden of brain and CNS cancer than women. This includes higher incidence, mortality, and DALYs. The reasons behind this difference are not fully understood but may involve biological factors, occupational exposures, and differences in healthcare utilization.
Encouraging Trends in Young Children
One bright spot in the data involves children under the age of five, who showed a sharp decline in cancer incidence. This trend may reflect improvements in prenatal care, early childhood health interventions, or environmental protections, though more research is needed to confirm the underlying causes.
Rising Risk in Older Adults
At the opposite end of the age spectrum, adults over 70 experienced increasing rates of both diagnosis and death from CNS cancers. As the U.S. population continues to age, this trend could place additional strain on healthcare systems, particularly in regions already facing shortages of specialists.
Socioeconomic Status Plays a Role
The study also examined outcomes through the lens of the Sociodemographic Index (SDI), which incorporates income, education, and fertility rates. Areas with lower SDI scores tended to have higher mortality and disease burden, reinforcing the idea that where you live and your access to resources can influence cancer outcomes as much as biology.
Why These Findings Matter for Policy and Healthcare
The researchers emphasize that these results are not just academic. Understanding who is most affected and where can help guide:
- Targeted healthcare funding
- Improved access to specialized cancer care
- Updates to clinical guidelines
- Public health initiatives focused on underserved regions
As medical knowledge evolves, clinical practices and health policies must evolve with it. Without actively examining long-term data, systemic disparities can remain hidden in plain sight.
A Closer Look at the Global Burden of Disease Approach
The Global Burden of Disease framework is particularly valuable because it allows researchers to compare diseases across regions and time periods using consistent methods. Rather than focusing only on survival, it captures how conditions affect daily life, productivity, and long-term wellbeing.
For CNS cancers, this approach highlights a critical reality: living longer does not always mean living better, and reducing disability is just as important as reducing death rates.
What This Study Does Not Answer Yet
Despite its scale, the study does not pinpoint specific environmental or genetic causes behind regional differences. It also does not distinguish in detail between different types of brain tumors, which can vary widely in aggressiveness and treatment response. These gaps point toward the need for future research focused on tumor subtypes, environmental exposure, and healthcare delivery models.
Looking Ahead
Overall, the findings present a mixed picture. On one hand, fewer people are dying and overall disability has declined, reflecting real progress in treatment and care. On the other hand, persistent geographic and socioeconomic disparities remain, and the steady incidence rate suggests that prevention strategies have not advanced at the same pace.
For clinicians, policymakers, and patients alike, this study serves as a reminder that medical progress is rarely evenly distributed. Understanding and addressing these differences will be essential if future gains are to benefit everyone, regardless of where they live.
Research Reference:
https://jamanetwork.com/journals/jamaneurology/fullarticle/2841027