AI Is Helping Doctors Predict Nutrition Risks for ICU Patients on Ventilators
Artificial intelligence is steadily finding its place in hospitals, and a new study suggests it could play a meaningful role in one of the most overlooked areas of critical care: nutrition for ICU patients on ventilators. Researchers from the Icahn School of Medicine at Mount Sinai have developed an AI-based system that can predict which critically ill patients are at risk of being underfed during the earliest and most crucial days of intensive care. The study was published online on December 17, 2025, in the journal Nature Communications.
This research focuses on patients who are mechanically ventilated, meaning they rely on machines to help them breathe. These patients often cannot eat normally and instead receive nutrition through enteral feeding, usually delivered through tubes. While feeding may sound straightforward, ensuring the right amount of nutrition at the right time is far more complex than it seems.
Why Nutrition in the ICU Matters So Much
The first week on a ventilator is especially critical. During this period, patients’ metabolic needs change rapidly due to stress, inflammation, infection, and the effects of medications. Even small gaps between what a patient needs and what they actually receive can add up quickly.
The study highlights a concerning reality: underfeeding is extremely common in ICUs. According to the researchers’ analysis, between 41% and 53% of patients were underfed by day three of ventilation. By day seven, 25% to 35% of patients were still not receiving enough nutrition. These numbers come from large ICU datasets in both Europe and the United States, showing that the problem is widespread and not limited to one healthcare system.
Underfeeding can lead to muscle loss, delayed recovery, weakened immune response, longer hospital stays, and worse overall outcomes. Despite this, nutrition is often pushed aside as clinicians focus on stabilizing breathing, blood pressure, infections, and organ function.
Introducing NutriSighT, an AI Tool Designed for ICU Nutrition
To tackle this issue, the Mount Sinai research team built an AI tool called NutriSighT. The name reflects its purpose: providing clearer insight into nutrition risks before they become serious problems.
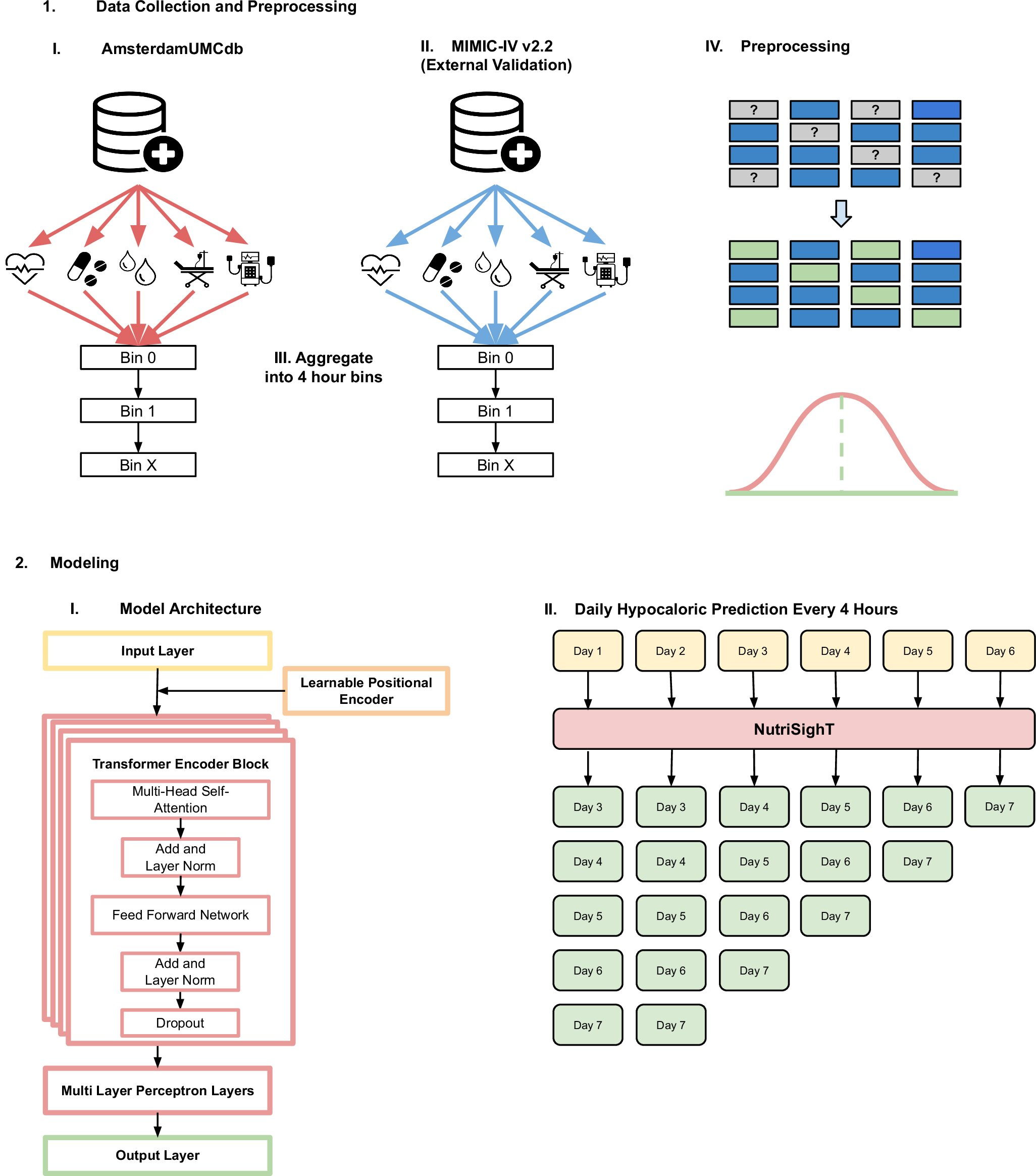
NutriSighT is an interpretable transformer-based AI model, a type of architecture commonly used in advanced AI systems that analyze sequences over time. Instead of looking at a single snapshot of patient data, the model continuously tracks changes and updates its predictions every four hours.
The AI analyzes routine ICU data, including:
- Vital signs such as blood pressure
- Laboratory values like sodium levels
- Medications, including sedation
- Feeding records and nutrition delivery
- Other standard clinical measurements already collected in ICUs
Using this information, NutriSighT predicts whether a patient is likely to be underfed on days 3 through 7 of mechanical ventilation, often hours in advance. This early warning could give clinicians time to adjust feeding strategies before deficits worsen.
What Makes This AI Model Different
One of the most important aspects of NutriSighT is that it is dynamic and interpretable. Many AI systems function like black boxes, offering predictions without explaining how they arrived at them. NutriSighT, however, highlights which specific factors are contributing to a patient’s risk.
For example, the model can show how changes in blood pressure, electrolyte levels, or sedation are influencing nutrition delivery. This transparency makes it far more useful in real clinical settings, where doctors and nutrition teams need to understand why a risk is increasing before they act.
The researchers emphasize that this tool is not meant to replace clinicians. Instead, it acts as a decision-support system, helping healthcare teams spot risks earlier and respond more effectively.
Data Sources and Model Performance
To build and validate NutriSighT, the research team used two major, deidentified ICU datasets:
- AmsterdamUMCdb, a large European ICU database
- MIMIC-IV, a widely used ICU database from the United States
Training and validation across different regions helped ensure that the model could perform well in diverse healthcare environments.
In terms of performance, NutriSighT showed strong predictive ability:
- An AUROC of 0.81 in internal validation
- An AUROC of 0.76 in external validation
- Strong precision-recall performance across datasets
The model also outperformed more traditional machine-learning approaches, such as XGBoost, particularly when it came to adapting to changing patient conditions over time.
How This Could Change ICU Care
The potential applications of NutriSighT go beyond simple predictions. The researchers suggest that the tool could:
- Support personalized feeding plans tailored to individual patients
- Help nutrition and ICU teams prioritize high-risk patients
- Inform the design of clinical trials focused on optimal nutrition strategies
- Serve as an early-warning system integrated into electronic health records
The ultimate goal is simple but powerful: delivering the right amount of nutrition to the right patient at the right time. If successful, this approach could improve recovery, reduce complications, and shorten ICU stays.
Next Steps for the Research
While the results are promising, the researchers are clear that more work lies ahead. The next phase includes prospective, multi-site clinical trials to test whether acting on NutriSighT’s predictions actually improves patient outcomes in real-world settings.
They also plan to explore deeper integration with hospital systems and expand the model to handle broader nutrition targets and patient populations. Careful implementation will be essential to ensure that AI complements clinical judgment rather than complicating it.
A Broader Look at AI and Nutrition in Critical Care
This study fits into a growing movement toward AI-driven personalized medicine. Nutrition has historically lagged behind other aspects of critical care when it comes to technological innovation. Tools like NutriSighT suggest that this may finally be changing.
AI excels at recognizing patterns across massive datasets, something humans struggle to do in fast-paced ICU environments. When applied thoughtfully, it can help clinicians stay ahead of problems instead of reacting after harm has already occurred.
At the same time, nutrition remains a deeply human aspect of care, closely tied to recovery, dignity, and quality of life. Combining clinical expertise with intelligent tools may be the key to finally giving ICU nutrition the attention it deserves.
Study and Publication Details
The study is titled “NutriSighT: Interpretable Transformer Model for Dynamic Prediction of Underfeeding Enteral Nutrition in Mechanically Ventilated Patients.”
It was published in Nature Communications (2025) and authored by Mateen Jangda, Jayshil Patel, Akhil Vaid, Jaskirat Gill, Paul McCarthy, Jacob Desman, Rohit Gupta, Dhruv Patel, Nidhi Kavi, Shruti Bakare, Eyal Klang, Robert Freeman, Anthony Manasia, John Oropello, Lili Chan, Mayte Suarez-Farinas, Alexander W. Charney, Roopa Kohli-Seth, Girish N. Nadkarni, and Ankit Sakhuja.
Research paper link:
https://www.nature.com/articles/10.1038/s41467-025-66200-1