AI-Powered Wearable From University of Arizona Aims to Transform Preventative Care for Older Adults
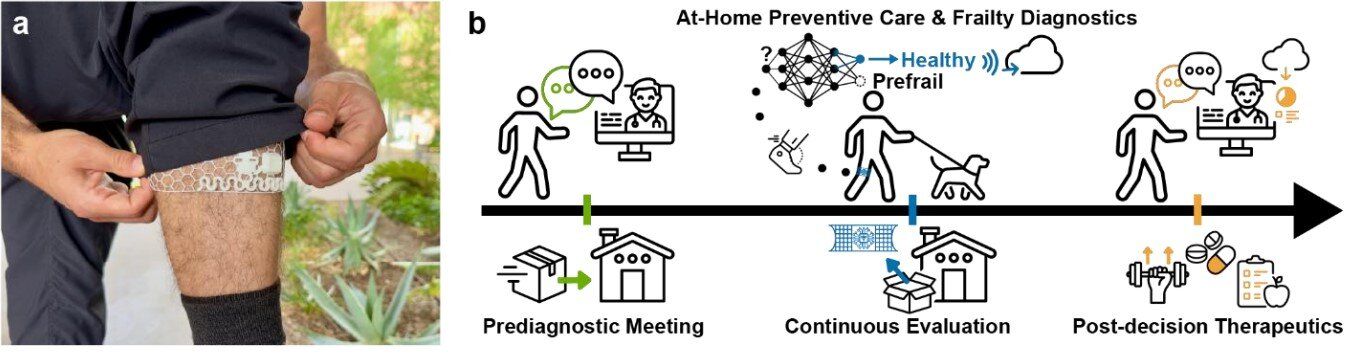
Researchers at the University of Arizona have developed a new AI-powered wearable device designed to detect early signs of frailty in older adults, a condition strongly linked to falls, disability, and hospitalization. Created by the Gutruf Lab within the university’s biomedical engineering department, this technology represents a significant move toward preventative, rather than reactive, elderly care.
Frailty is a gradual and often overlooked condition. In many healthcare systems today, assessments happen only after something serious occurs, such as a fall or a hospital admission. The newly developed wearable is intended to change that approach by continuously monitoring subtle changes in movement that may signal declining physical resilience long before a major incident occurs.
What the Wearable Does and How It Works
At the center of this research is a soft, mesh-based wearable sleeve that fits comfortably around the lower thigh. The sleeve is approximately two inches wide, lightweight, and produced using 3D-printing techniques. Embedded within the fabric are miniature motion sensors that track leg movement throughout everyday activities.
The device focuses on continuous gait monitoring, analyzing parameters such as leg acceleration, step variability, and movement symmetry. These factors are well-established indicators of physical decline and frailty, especially in older adults. Instead of relying on occasional clinical assessments, the sleeve collects data during real-world movement, providing a much more accurate picture of a person’s functional health.
What makes this wearable particularly notable is its use of on-device artificial intelligence, also known as Edge AI. Rather than transmitting massive amounts of raw motion data, the device processes information locally. Only the final analytical results are shared, which reduces data transmission by approximately 99%.
Why Edge AI Matters
Continuous movement tracking typically generates huge datasets. Uploading this information would normally require strong internet connectivity and frequent battery charging, making long-term use impractical. By performing AI analysis directly on the wearable, the researchers solved both problems at once.
The wearable sends only summarized results via Bluetooth to a nearby smart device, such as a phone or tablet. This approach drastically reduces power consumption and removes the need for high-speed internet connections. As a result, the device is particularly well suited for remote patient monitoring, including use in rural or under-resourced communities where reliable broadband access may be limited.
To further support ease of use, the sleeve includes long-range wireless charging, eliminating the need for users to plug in the device or replace batteries frequently. This design choice is especially important for older adults, for whom complex charging routines can become a barrier to consistent use.
Why Frailty Detection Is So Important
Frailty is more than just weakness. It reflects a reduced ability of the body to recover from stress, making individuals more vulnerable to falls, illness, and hospitalization. According to prior research, about 15% of U.S. adults aged 65 and older are affected by frailty, and the risk increases with age.
Currently, frailty is often identified too late. Traditional assessments may involve short walking tests, grip strength measurements, or questionnaires performed during clinic visits. These methods offer only a snapshot of a person’s health and can miss gradual declines that occur over weeks or months.
By enabling continuous, high-fidelity monitoring, the AI-powered sleeve allows clinicians to detect changes earlier and intervene sooner. Early intervention could include physical therapy, balance training, medication adjustments, or lifestyle changes that help prevent serious outcomes.
Design Philosophy Behind the Device
Comfort and discretion were central to the device’s design. The research team aimed to create something that users would forget they were wearing. The soft mesh structure, flexible materials, and adhesive-free fit help minimize skin irritation and discomfort during long-term use.
The wearable is described as being effectively “invisible” under clothing, which may improve adherence and acceptance among older adults. This is a crucial factor, as even the most advanced health technology is ineffective if people are unwilling to wear it consistently.
The Gutruf Lab has spent several years developing wearable technologies for health monitoring. Earlier work from the lab included an adhesive-free wearable that measured water vapor and skin gases to track physiological stress. The frailty detection sleeve builds on this foundation, adapting prior sensor and materials research to address mobility and aging.
Validation and Research Findings
The study introducing this wearable was published in Nature Communications under the title “Wearable AI for on-device frailty assessment.” The research demonstrated that the sleeve’s gait measurements closely aligned with established clinical assessments used to evaluate frailty.
During testing, participants wore the device for extended periods, allowing researchers to collect and analyze real-world walking data. The AI models embedded in the wearable were able to identify patterns associated with frailty with high accuracy, while maintaining extremely low power consumption.
Another key outcome was the device’s ability to operate for long durations without user intervention. This reliability is essential for real-world deployment, particularly in populations where frequent device management may be challenging.
Broader Implications for Healthcare
This wearable reflects a growing shift toward patient-centered, decentralized healthcare. By placing advanced diagnostic capabilities directly on the body, clinicians can monitor health continuously rather than relying solely on clinic visits.
Such technology has the potential to reduce healthcare costs by preventing falls and hospital admissions, which are among the most expensive and dangerous outcomes for older adults. It may also help healthcare providers allocate resources more efficiently by identifying individuals who need intervention earlier.
Importantly, the low data and power requirements make the device accessible beyond major urban medical centers. This could help address healthcare disparities by bringing advanced monitoring tools to populations that are often underserved.
What Comes Next
While the results are promising, the researchers emphasize that further studies are needed. Larger clinical trials involving more diverse populations will be required before the device can be widely adopted or commercialized. Regulatory approval and long-term safety evaluations will also be necessary.
Still, the concept demonstrates how AI-driven wearables can move healthcare toward a more preventative and proactive model, particularly for aging populations.
Understanding Frailty and Gait Monitoring
Frailty often manifests subtly through changes in walking patterns. Reduced stride length, increased variability, and asymmetry between steps can all indicate declining neuromuscular control. Gait analysis has long been used in research settings, but wearable technology now makes it possible to apply these insights continuously in daily life.
By combining biomechanics, machine learning, and wearable engineering, this research highlights how interdisciplinary approaches can address complex health challenges. As populations continue to age globally, such innovations may play a key role in maintaining independence and quality of life for older adults.
Research Paper:
https://www.nature.com/articles/s41467-025-67728-y