Behavioral Health Now Accounts for 40 Percent of All Children’s Health Spending in the U.S., Nearly Doubling in a Decade

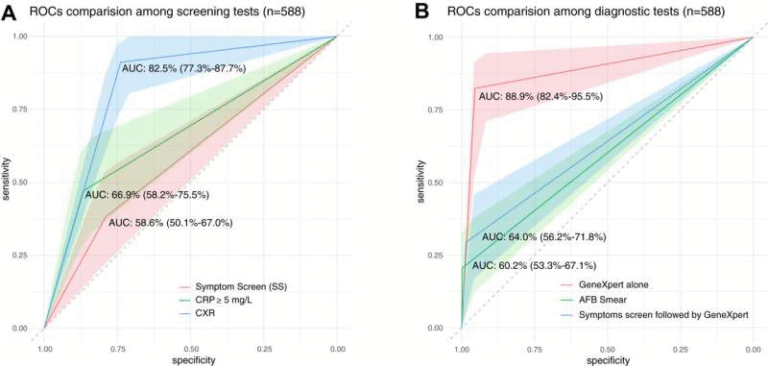
Behavioral health care has quietly become one of the largest drivers of medical spending for children in the United States, and the numbers behind this shift are striking. A new study published in JAMA Pediatrics reveals that by 2022, behavioral health services accounted for 40 percent of all medical expenditures for U.S. children, nearly doubling from 22 percent in 2011. This change reflects not only rising demand for mental and behavioral health care among young people, but also growing financial pressure on families trying to access that care.
The study focuses on children aged 6 to 17 years and analyzes nationally representative spending data from 2011 through 2022. Over that period, total pediatric behavioral health spending climbed to $41.8 billion in 2022 alone. Of that amount, families paid $2.9 billion out-of-pocket, a figure that has raised significant concerns among clinicians, researchers, and policymakers alike.
What makes this trend especially concerning is not just how much is being spent, but who is bearing the cost. The study found that out-of-pocket expenses for children’s behavioral health care have been increasing much faster than spending for other types of medical care, placing a disproportionate burden on families.
Behavioral Health Costs Are Rising Faster Than Other Medical Expenses
One of the clearest findings from the study is the difference in growth rates between behavioral and non-behavioral health spending. Between 2011 and 2022, out-of-pocket spending for pediatric behavioral health increased by an average of 6.4 percent per year. In contrast, out-of-pocket spending for non-behavioral health medical care grew at a much slower rate of 2.7 percent annually.
By 2022, more than one-quarter of all pediatric out-of-pocket health care spending was directed toward behavioral health services. This shift signals that families are increasingly paying directly for mental health-related care, even as insurance coverage expands in theory.
The rapid growth in out-of-pocket costs suggests that insurance plans may not be keeping pace with children’s behavioral health needs. Many families are forced to seek care outside of their insurance networks due to provider shortages, long wait times, or limited coverage options. When that happens, families often face higher deductibles, co-pays, and full out-of-pocket payments.
The Financial Burden on Families Is Significant
The study also highlights the real-world financial strain these costs create. Researchers found that 1 in 21 U.S. families experiences extreme financial burden due to out-of-pocket health care costs. In this context, extreme financial burden is defined as spending more than 10 percent of household income on health care expenses.
Families with at least one child receiving behavioral health services were found to be about 40 percent more likely to experience this level of financial strain compared to families without such care needs. This finding underscores how mental and behavioral health care, while essential, can significantly disrupt household finances.
These pressures can influence difficult family decisions, such as delaying care, reducing the frequency of visits, or avoiding treatment altogether. Over time, those delays can worsen mental health conditions and lead to more complex and costly interventions later on.
How and Where Children Receive Behavioral Health Care Is Changing
Beyond overall spending, the study sheds light on major shifts in how behavioral health care is delivered to children.
Spending increased sharply in several key areas:
- Home health care spending for pediatric behavioral health grew by approximately 25 percent per year, reflecting expanded use of in-home services and community-based care.
- Outpatient in-person visits increased by around 11 percent per year, indicating sustained demand for traditional therapy and counseling services.
- Outpatient telehealth visits saw the most dramatic change, increasing by an astonishing 99 percent per year between 2020 and 2022.
The explosion in telehealth use coincided with the COVID-19 pandemic, when in-person services became limited and virtual care options expanded rapidly. Even after pandemic-related restrictions eased, telehealth remained a critical part of behavioral health delivery for children and adolescents.
Telehealth has helped improve access, especially for families in rural or underserved areas. However, the study points out that gaps in reimbursement and regulatory barriers continue to limit its full potential. Differences in state licensing rules and inconsistent insurance reimbursement rates can make it difficult for families to rely on telehealth as a stable, affordable option.
Insurance Coverage and Parity Remain Ongoing Challenges
A recurring theme throughout the study is the mismatch between children’s behavioral health needs and existing insurance structures. Despite mental health parity laws that require insurance coverage for behavioral health services to be comparable to coverage for physical health care, many families still encounter limited provider networks and inadequate coverage.
The study emphasizes the need for stronger state-level insurance parity laws and better enforcement of existing regulations. Without these changes, families will likely continue to face high out-of-pocket costs, even when they have insurance coverage on paper.
Improving provider networks, increasing reimbursement rates, and ensuring that behavioral health services are treated equally within insurance plans are seen as critical steps toward reducing the financial burden on families.
Understanding Pediatric Behavioral Health Care
Behavioral health care for children includes a wide range of services addressing emotional, psychological, and behavioral challenges. These can include treatment for anxiety disorders, depression, attention-deficit/hyperactivity disorder (ADHD), behavioral disorders, and substance use issues, among others.
Over the past decade, awareness and diagnosis of these conditions have increased. Schools, pediatricians, and families are more likely to recognize symptoms and seek help earlier. While this increased awareness is a positive development, it also contributes to higher demand for services that the current health care system may not be fully equipped to handle.
Why This Trend Matters Long Term
The findings from this study offer a clear snapshot of a broader youth behavioral health crisis. Rising spending reflects both increased need and systemic gaps in care delivery and coverage. Without meaningful policy changes, families may continue to shoulder growing costs, and disparities in access to care could widen.
At the same time, the data also show where progress is being made. Expanded outpatient services, increased home-based care, and the rapid adoption of telehealth all point toward a more flexible and accessible behavioral health system. The challenge moving forward will be ensuring that these services are affordable, equitable, and sustainable for families across income levels.
Research Reference:
Expenditures for Pediatric Behavioral Health Care Over Time and Estimated Family Financial Burden, JAMA Pediatrics (2025)
https://jamanetwork.com/journals/jamapediatrics/fullarticle/2815181