Brain Immune Cells May Be Causing More Alzheimer’s Damage in Women Than Men

Alzheimer’s disease affects more than 7 million Americans, and one of the most striking statistics surrounding the condition is that nearly two-thirds of patients are women. For years, scientists have known about this imbalance, but the biological reasons behind it have remained frustratingly unclear. New research is now offering an important clue, pointing toward the brain’s own immune cells as a possible driver of greater damage in females.
Researchers from the University of Rochester’s Del Monte Institute for Neuroscience, led by neuroscientist M. Kerry O’Banion, have found that microglia, the immune cells of the brain, behave differently in female brains affected by Alzheimer’s disease. Their findings suggest that these differences may contribute to more severe neuronal damage in females compared to males.
Understanding Microglia and Their Role in Alzheimer’s Disease
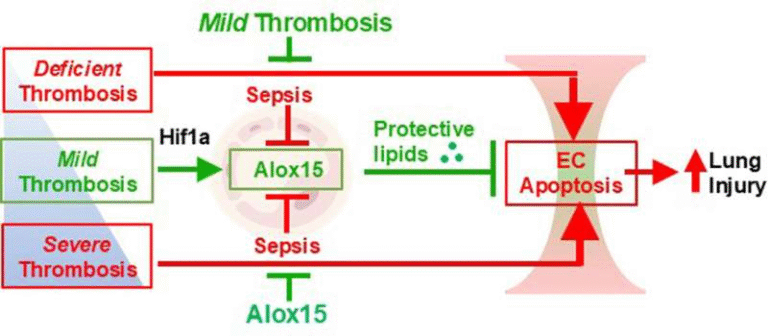
Microglia play a vital role in maintaining brain health. In a healthy nervous system, they help clear debris, protect neurons from infection, and support normal brain function. However, in Alzheimer’s disease, microglia are drawn toward amyloid-β plaques, the sticky protein clumps that accumulate between neurons and are one of the hallmarks of the disease.
While microglia are supposed to help by clearing these plaques, their response can sometimes backfire. Instead of protecting neurons, they can trigger chronic inflammation, which worsens brain damage over time. The new study shows that this inflammatory response is not the same in males and females.
Stronger Interferon Signaling in Female Microglia
Using a widely studied Alzheimer’s mouse model known as 5xFAD mice, the researchers closely examined how microglia respond to amyloid-β plaques. What they found was striking: female microglia expressed significantly higher levels of interferon-related genes compared to male microglia.
Interferons are signaling molecules best known for their role in fighting viral infections. When cells detect viral DNA or RNA, interferon signaling helps trigger immune defenses. However, in the context of Alzheimer’s disease, the role of interferons is still poorly understood.
Previous studies have shown that interferon signaling can drive neuroinflammation and contribute to synaptic damage, meaning it can harm the connections between neurons. The new findings suggest that female microglia may be more prone to activating this pathway, potentially amplifying brain damage.
One hypothesis proposed by the researchers is that when microglia consume amyloid-β plaques, they may encounter fragments of DNA or RNA and mistakenly interpret them as viral material. This could trigger an unnecessary interferon response, even though no virus is present.
Plaque Shape and Structure Differ Between Sexes
The study did not just examine gene expression. Researchers also looked closely at the physical characteristics of amyloid-β plaques. They discovered that female microglia tend to leave behind larger and more irregularly shaped plaques after interacting with them.
These irregular plaques were associated with greater neuritic dystrophy, a form of damage that affects neuronal projections such as axons and dendrites. In simple terms, the plaques left behind in female brains appeared to disrupt more neuronal connections than those found in male brains.
This suggests that even though microglia in females may be actively engaging with plaques, the end result could be more structural damage rather than effective cleanup.
Hormones Are Likely Not the Explanation
One common assumption in Alzheimer’s research has been that hormonal differences, particularly fluctuations in estrogen, might explain why women are more affected. Interestingly, this study challenges that idea.
The researchers analyzed female mice at different stages of their estrous cycle, which mirrors hormonal changes similar to the menstrual cycle in humans. They found no significant differences in amyloid-β pathology or microglial gene expression across these stages.
This indicates that short-term hormonal fluctuations are unlikely to be the main driver of the observed sex differences. Instead, the findings suggest that male and female microglia may be inherently different at a biological level.
Why These Findings Matter for Alzheimer’s Treatment
Microglia are already known to play a central role in the progression and severity of Alzheimer’s disease, but this study highlights that their impact may be sex-specific. If female microglia are more likely to activate damaging interferon pathways, this could help explain why women often experience faster disease progression or greater cognitive decline.
These insights open the door to personalized treatment strategies. Rather than assuming Alzheimer’s affects everyone in the same way, future therapies could be tailored based on biological sex. For example, targeting interferon signaling pathways in microglia might be especially beneficial for female patients.
Researchers are now focused on determining whether these sex-based differences exist in humans and whether modifying microglial behavior can alter the course of the disease.
What We Know About Sex Differences in Alzheimer’s Disease
Beyond this specific study, a growing body of research supports the idea that Alzheimer’s disease is not a one-size-fits-all condition.
Some key observations include:
- Women are more likely to develop Alzheimer’s disease than men, even after accounting for longer lifespan.
- Female brains often show different patterns of inflammation and immune activation.
- Microglia are known to differ between sexes even in healthy brains, suggesting baseline biological differences.
Together, these findings reinforce the idea that sex should be treated as a critical variable in neuroscience research, particularly when studying neurodegenerative diseases.
The Bigger Picture: Neuroinflammation and Brain Health
Neuroinflammation is increasingly recognized as a major factor in Alzheimer’s disease. While inflammation is a natural and necessary immune response, chronic inflammation in the brain can accelerate neuronal loss and cognitive decline.
Microglia sit at the center of this process. Understanding when they protect the brain and when they cause harm is one of the biggest challenges in modern neuroscience. This study adds an important layer by showing that sex differences in immune signaling may shape how Alzheimer’s unfolds over time.
Looking Ahead
The findings from the University of Rochester team represent a significant step toward understanding why Alzheimer’s disease affects women so disproportionately. By uncovering sex-specific immune responses in the brain, researchers are moving closer to treatments that reflect the biological realities of patients rather than relying on generalized approaches.
While more work is needed to confirm these mechanisms in humans, the study provides a compelling framework for future research and drug development. It also underscores the importance of studying male and female biology separately, especially in diseases as complex and devastating as Alzheimer’s.
Research Paper Reference:
https://link.springer.com/article/10.1186/s12974-025-03659-1