CAR T-Cell Therapy Helps Aging Intestines Heal Faster and Restore Gut Health in Mice
As people grow older, it’s common to notice that digestion isn’t quite what it used to be. Foods that were once easy to handle can suddenly cause discomfort, bloating, or inflammation. Scientists have long suspected that this change has a lot to do with the intestinal epithelium, a thin but vital layer of cells lining the gut. Now, researchers from Cold Spring Harbor Laboratory (CSHL) have found a surprising way to rejuvenate this aging tissue using CAR T-cell therapy, a treatment best known for fighting cancer.
The study, published in Nature Aging, shows that engineered immune cells can dramatically improve intestinal repair and function in aging mice. Even more striking, a single treatment produced long-lasting benefits that persisted for up to a year. This work opens the door to future therapies aimed at improving gut health in elderly individuals and in patients whose intestines have been damaged by cancer treatments.
Why the Intestinal Epithelium Matters So Much
The intestinal epithelium is a single-cell-thick lining that performs several essential tasks. It absorbs nutrients, forms a protective barrier against harmful bacteria, and plays a key role in immune regulation. Under healthy conditions, this layer is constantly renewing itself, fully regenerating every three to five days.
However, aging and external damage can disrupt this rapid renewal. When regeneration slows or stops, the intestinal barrier weakens. This can lead to chronic inflammation, poor nutrient absorption, and conditions such as leaky gut syndrome, where harmful substances pass from the intestine into the bloodstream.
Radiation therapy, especially for pelvic or abdominal cancers, can make this problem worse by directly damaging epithelial cells. Many cancer survivors struggle with long-term digestive issues as a result.
The Role of Senescent Cells in Aging Guts
One major reason intestinal regeneration declines with age is the accumulation of senescent cells. These cells are no longer able to divide, but instead of dying off, they linger in tissues. Over time, they release inflammatory signals and interfere with nearby healthy cells.
Senescent cells have been linked to a wide range of age-related diseases, including diabetes, neurodegeneration, and tissue degeneration. In the gut, they disrupt stem cell function and prevent effective repair of the epithelial lining.
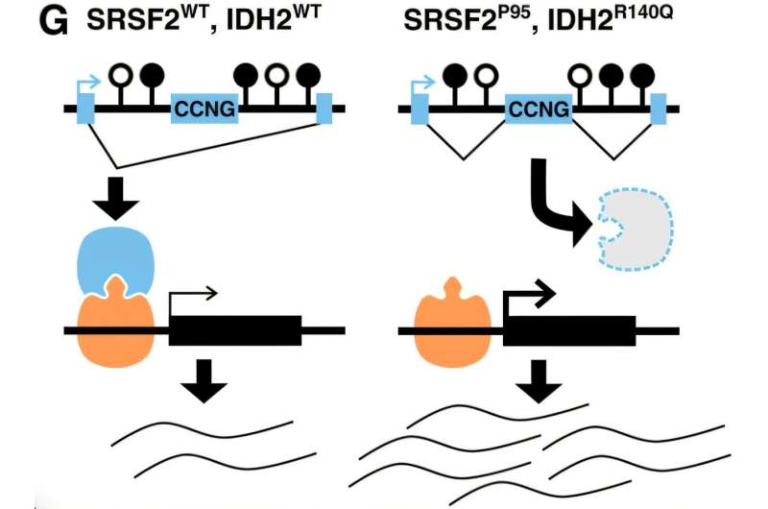
A key marker found on many senescent cells is uPAR (urokinase plasminogen activator receptor). In this study, researchers observed that epithelial cells in aged human intestines frequently tested positive for uPAR and showed reduced levels of p21, a tumor suppressor protein normally involved in regulating cell growth.
Using CAR T-Cell Therapy Beyond Cancer
CAR T-cell therapy involves modifying a patient’s immune cells so they can recognize and destroy specific targets. It has already transformed treatment for certain blood cancers. At CSHL, Assistant Professor Corina Amor Vegas and her lab have been exploring whether this approach could also be used to eliminate senescent cells.
In earlier work, Amor Vegas and her team engineered anti-uPAR CAR T cells and showed that these cells could selectively remove senescent cells in mice, leading to major improvements in metabolic health. The new study asked an important follow-up question: could the same strategy rejuvenate the aging intestine?
To find out, Amor Vegas teamed up with Assistant Professor Semir Beyaz and graduate student Onur Eskiocak. Together, they tested the effects of uPAR-targeting CAR T cells on the intestines of both young and old mice.
Clear Improvements in Gut Function and Healing
The results were consistent and striking. Mice treated with anti-uPAR CAR T cells showed significant improvements regardless of age. Their intestines absorbed nutrients more effectively, inflammation levels dropped, and the epithelial lining regenerated much faster after injury.
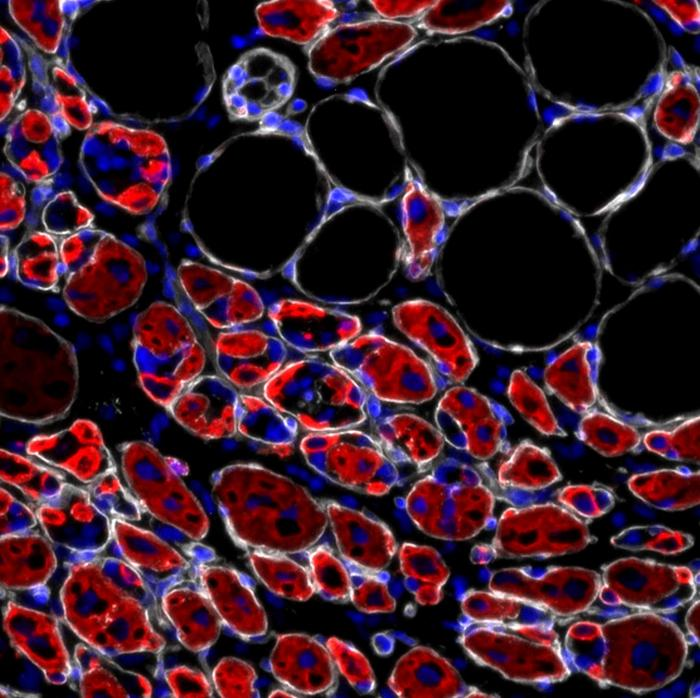
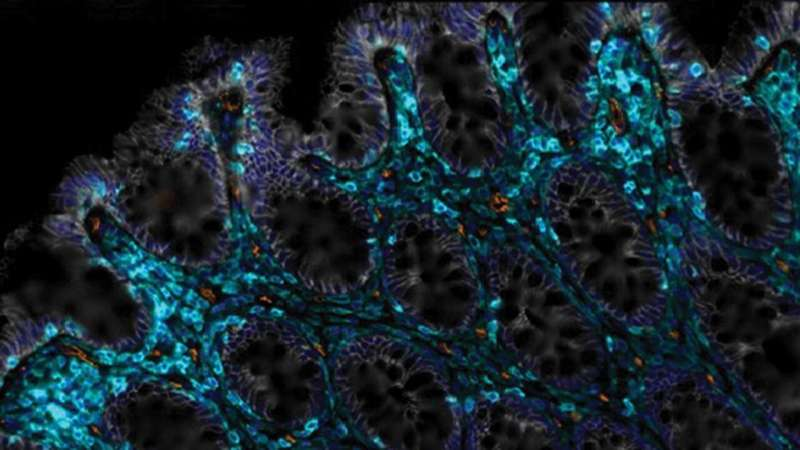
Microscopic analysis revealed several key changes. Treated intestines had far fewer uPAR-positive cells, indicating a reduction in senescent cell burden. At the same time, there was a noticeable increase in healthy intestinal stem cells, which are essential for continuous renewal of the gut lining.
Importantly, these benefits were not short-lived. A single administration of CAR T cells improved gut health for at least one full year, a remarkable outcome in aging research.
Protection Against Radiation-Induced Gut Damage
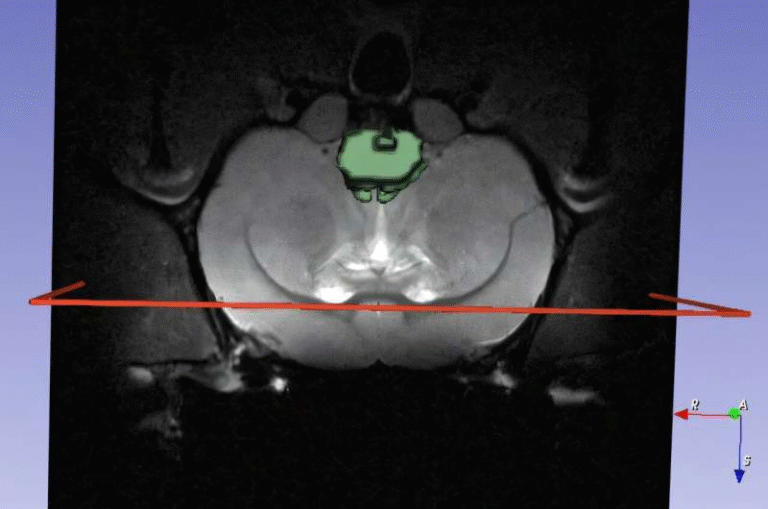
The team also looked at how CAR T-cell therapy might help in situations that mimic real-world medical challenges. To simulate the effects of cancer radiation therapy, the researchers irradiated the epithelial cells in mice.
Radiation typically causes severe damage to the intestinal lining, leading to prolonged inflammation and impaired healing. In this study, mice that received CAR T-cell treatment recovered far more effectively than untreated animals. Their intestinal tissue regenerated faster, and long-term damage was significantly reduced.
This finding is especially relevant for cancer patients, many of whom develop chronic gut issues after radiation therapy.
Evidence Supporting Human Relevance
While the experiments were conducted in mice, the researchers also examined human intestinal and colorectal cells. They found strong evidence that anti-uPAR CAR T cells can promote regeneration in these human cells as well.
Although the exact mechanisms are still being studied, the presence of uPAR on aging human intestinal cells suggests that this approach could one day translate into human therapies. Much more work is needed before clinical trials can begin, but the results provide an encouraging foundation.
Why Targeting Senescent Cells Is So Promising
This study adds to a growing body of evidence that senescent cells are not just a byproduct of aging, but an active driver of tissue decline. By selectively removing these cells, it may be possible to restore normal function without disrupting healthy tissue.
CAR T-cell therapy offers a level of precision that traditional drugs often lack. Instead of broadly suppressing inflammation or stimulating growth, it directly removes the cells that are causing the problem.
Challenges and Future Directions
Despite the excitement, CAR T-cell therapy is not without risks. In cancer patients, it can cause serious side effects if immune activation becomes excessive. Any future application for aging or gut health will require careful control, dosing strategies, and extensive safety testing.
Researchers are also working to better understand how eliminating senescent cells leads to increased stem cell activity and long-term tissue repair. Answering these questions will be crucial for designing safe and effective treatments for humans.
What This Means for the Future of Gut Health
This research represents an important step toward therapies that do more than manage symptoms. Instead of treating digestive problems with diet changes or anti-inflammatory drugs alone, future treatments may directly restore the gut’s natural ability to heal itself.
For elderly individuals, cancer survivors, and others with chronic intestinal damage, this approach could eventually improve quality of life in a meaningful way. While human applications are still years away, the science behind them is rapidly advancing.
Research paper reference:
https://www.nature.com/articles/s43587-025-01022-w