Discovery Reveals How the Keto Diet Can Prevent Seizures When Drugs Fail
For nearly a century, doctors have known that the ketogenic diet can dramatically reduce seizures in people with epilepsy who do not respond to medication. What they have not fully understood—until now—is how this high-fat, low-carbohydrate diet actually works inside the brain. New research from the University of Virginia School of Medicine has finally uncovered the biological mechanism behind this long-standing medical mystery, opening the door to potential treatments that could deliver the benefits of keto without the extreme dietary restrictions.
The study, published in Annals of Neurology, explains how the keto diet changes brain activity at a cellular level and why it is especially effective for drug-resistant epilepsy. Even more intriguing, the findings suggest possible implications for other neurological and neurodegenerative disorders, including Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and autism.
Why the Keto Diet Has Always Been a Medical Curiosity
The ketogenic diet was introduced as a therapy for epilepsy in the 1920s, long before modern anti-seizure medications existed. By sharply reducing carbohydrates and increasing fat intake, the body is forced to switch from using glucose to burning fat for energy. This metabolic shift leads to the production of molecules called ketone bodies, which the brain can use as an alternative fuel source.
Over the decades, doctors observed that many patients—particularly children with severe epilepsy—experienced fewer and less intense seizures while on the diet. However, despite its success, the diet is notoriously difficult to follow. It is extremely restrictive, often eliminating bread, rice, fruits, sweets, and many comfort foods. Side effects such as gastrointestinal distress, fatigue, and nutrient imbalances are also common.
Because of these challenges, researchers have long hoped to find a way to replicate keto’s benefits without requiring patients to stay on the diet. That goal is now much closer to reality.
The Breakthrough: A Receptor That Calms the Brain
The UVA research team, led by Jaideep Kapur, focused on one specific ketone produced during ketosis: β-hydroxybutyrate. This ketone is one of the most abundant molecules generated when the body burns fat instead of carbohydrates.
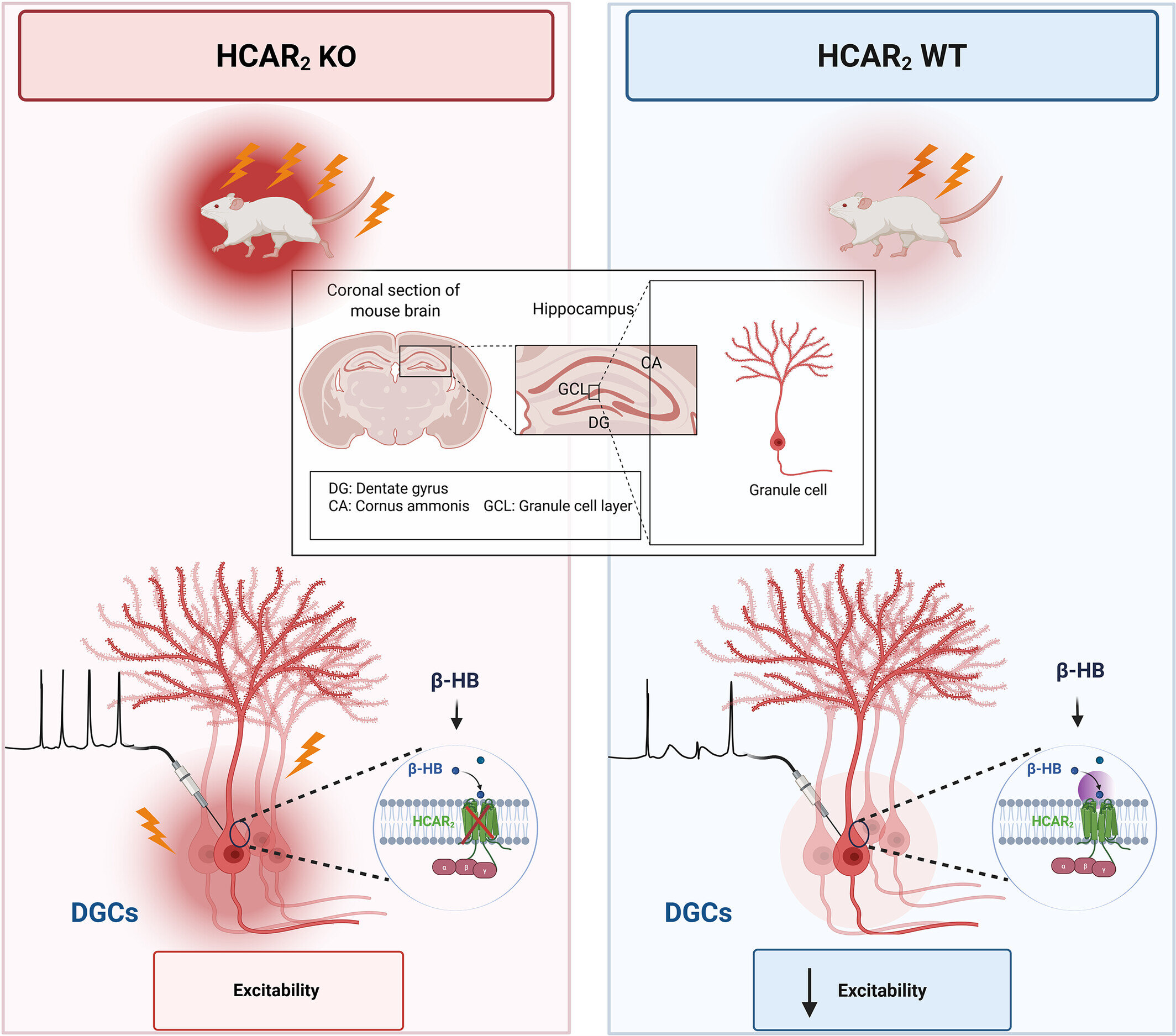
The researchers discovered that β-hydroxybutyrate interacts with a specific receptor in the brain called Hydroxycarboxylic Acid Receptor 2 (HCAR2). This receptor plays a critical role in regulating how brain cells communicate.
When β-hydroxybutyrate activates HCAR2, it reduces the excitability of neurons. This is a crucial finding because seizures occur when neurons become overly excitable and start firing uncontrollably. By calming these cells, the keto diet effectively lowers the brain’s tendency to produce seizures.
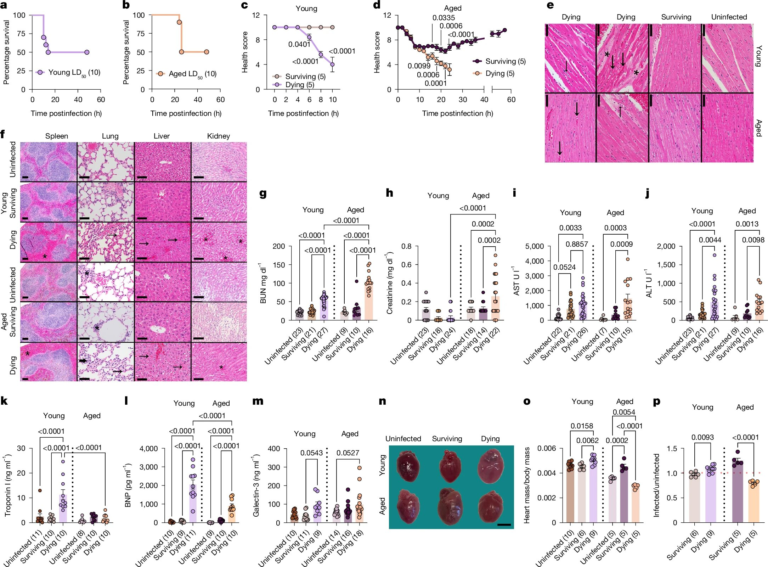
In laboratory studies using mice, the researchers showed that when HCAR2 was absent or nonfunctional, the anti-seizure effects of β-hydroxybutyrate disappeared. This confirmed that HCAR2 is essential to keto’s protective action.
Where This Happens in the Brain
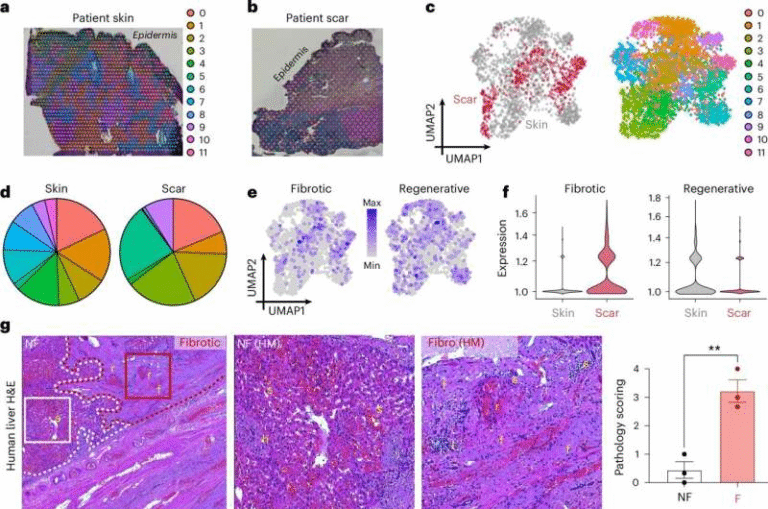
The team mapped where HCAR2 is located and found it concentrated in the hippocampus, a region of the brain where seizures commonly originate. The receptor was especially abundant in a specific type of cell already known to be involved in seizure activity.
HCAR2 was also found in microglia, the immune cells of the brain. Microglia play a key role in inflammation and immune defense within the nervous system. This suggests that the keto diet may influence seizures not only by calming neurons directly, but also by modulating immune responses in the brain.
This dual role—affecting both neurons and immune cells—helps explain why keto may have broader neurological benefits beyond epilepsy.
Why This Matters for Drug-Resistant Epilepsy
About one-third of people with epilepsy do not respond adequately to existing anti-seizure medications. For these patients, treatment options are limited, and seizures can severely impact quality of life.
The discovery of the HCAR2 pathway provides a clear molecular target for future therapies. Instead of forcing patients to follow a rigid, high-fat diet, scientists may be able to develop drugs that activate the same receptor and produce similar brain-calming effects.
One promising candidate already exists: niacin, also known as vitamin B3. Niacin is an FDA-approved drug commonly used to lower cholesterol, and it also activates HCAR2. Early experiments in mice suggest it may mimic some of the anti-seizure benefits of the keto diet, though much more research is needed to determine whether this translates to humans.
Potential Links to Other Brain Disorders
The implications of this research extend far beyond epilepsy. Neuronal hyperactivity—the same problem that triggers seizures—is also seen in the early stages of Alzheimer’s disease, as well as in conditions like autism and Parkinson’s disease.
Because HCAR2 is involved in regulating both neuron activity and brain immune responses, targeting this receptor could potentially help address neuroinflammation and abnormal signaling seen in these disorders. The researchers are now investigating how HCAR2 influences microglia and whether this pathway could be used to treat diseases such as multiple sclerosis and Alzheimer’s.
A Closer Look at Ketones and Brain Energy
Ketones are often discussed in the context of weight loss, but their role in brain function is far more complex. The brain normally relies on glucose for energy, but during fasting or ketosis, it can efficiently switch to ketones.
β-hydroxybutyrate is not just a fuel source—it also acts as a signaling molecule, influencing gene expression, inflammation, and neurotransmitter release. This study adds another layer to that understanding by showing how ketones directly affect brain receptors involved in seizure control.
This helps explain why the ketogenic diet has such a unique and powerful neurological impact compared to standard dietary approaches.
The Bigger Picture
This research finally provides a scientific explanation for a therapy that has worked in practice for decades. It validates the experiences of patients and clinicians who have relied on the ketogenic diet when medications failed, while also pointing toward a future where those benefits could be delivered in a safer, more accessible way.
For people with epilepsy who struggle to maintain the keto diet, and for those with other neurological conditions linked to brain hyperactivity, this discovery represents a major step forward.
As research continues, HCAR2 may become a central focus in the development of new treatments that harness the power of metabolism to protect and stabilize the brain.
Research Paper:
Hydroxycarboxylic Acid Receptor 2 Mediates β-hydroxybutyrate’s Antiseizure Effect in Mice, Annals of Neurology (2025)
https://doi.org/10.1002/ana.78098