How Circadian Rhythms Can Boost Infection Recovery and What It Means for Modern Healthcare
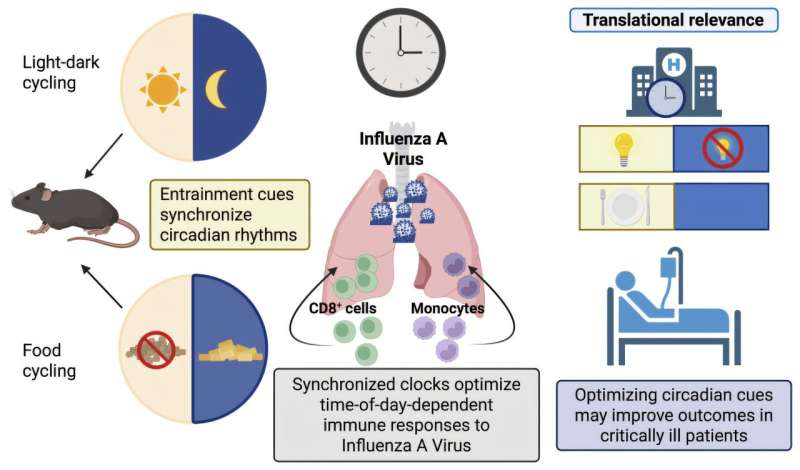
Researchers at Children’s Hospital of Philadelphia (CHOP) have uncovered compelling evidence that the body’s circadian rhythms, often described as internal biological clocks, play a critical role in how well individuals recover from viral infections such as influenza. The findings, published in the Journal of Clinical Investigation, add to a growing body of research suggesting that when and how the body experiences environmental cues like light and meals can significantly shape immune responses and recovery outcomes.
Circadian rhythms are natural, internal processes that follow an approximately 24-hour cycle. They evolved to help living organisms adapt to predictable changes in the environment, most notably the cycle of day and night. While many people associate circadian rhythms mainly with sleep, these rhythms influence nearly every biological function, from hormone release and metabolism to immune activity. Importantly, individual organs and even individual cells maintain their own clocks, all coordinated by circadian timing signals.
Most adults are already familiar with the effects of circadian disruption. Jet lag, night-shift work, and irregular sleep schedules are well known to reduce alertness, impair sleep quality, and negatively affect overall health. What is far less widely understood, however, is that the outcome of infections themselves can be directly influenced by the state of a person’s circadian rhythms. This is the central insight driving the CHOP research team’s latest study.
Circadian Timing and the Immune Response
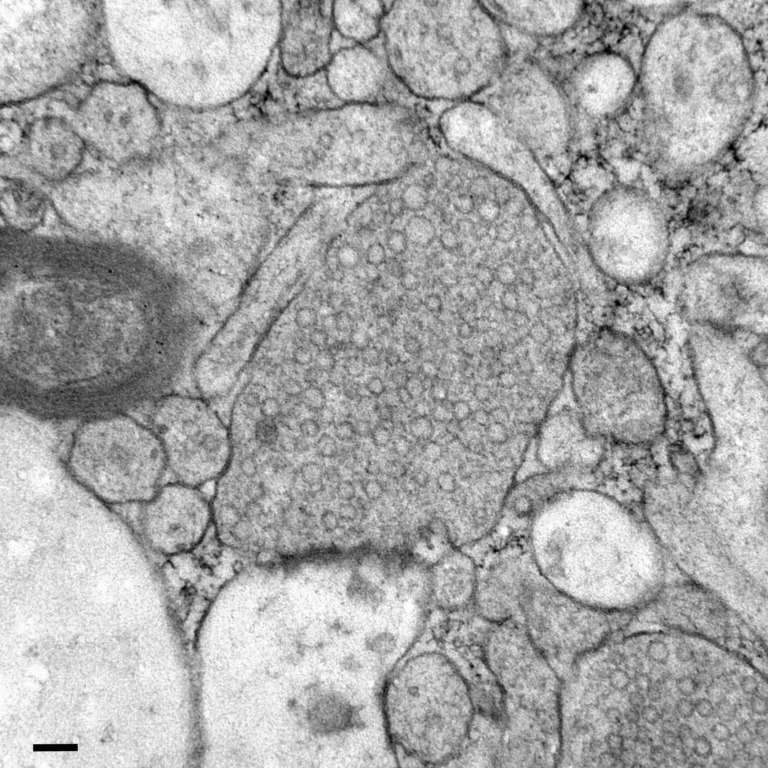
The immune system does not operate at a constant level throughout the day. Instead, immune cells, inflammatory signaling, and antiviral defenses fluctuate according to circadian timing. Previous research by the same team showed that the time of day at which an infection occurs can influence disease severity. In preclinical models of influenza, infections that began during certain times of the day resulted in better immune protection and improved outcomes.
What remained unclear was whether these benefits depended solely on the time of infection or whether they required the continued presence of rhythmic environmental cues after infection had already begun. Since influenza infections unfold over several days, the researchers were able to explore how circadian signals influence recovery well beyond the initial exposure to the virus.
The Role of Zeitgebers
Central to this study is the concept of zeitgebers, a German term meaning “time-givers.” Zeitgebers are external cues that help synchronize internal clocks across the body. The two most powerful zeitgebers for humans are light exposure and meal timing. Light primarily influences the master clock in the brain, while meals act as strong timing signals for metabolic and immune clocks in peripheral organs.
In controlled preclinical experiments, the researchers examined what happens when these cues are disrupted after infection. They found that disrupting environmental light cycles, effectively throwing off a normal rest–activity schedule, eliminated the time-of-day-specific protection seen in earlier studies. This disruption occurred within a critical window of vulnerability after infection and led to significantly worse outcomes.
Specifically, the immune response became dysregulated. Inflammatory immune cells accumulated excessively in the lungs during upper respiratory infection, worsening inflammation rather than resolving it. This overactive response is particularly concerning because lung inflammation is a major driver of severe illness in influenza and other respiratory viral infections.
Meal Timing as a Protective Factor
One of the most striking findings of the study was that maintaining a rhythmic meal schedule could partially counteract the harmful effects of disrupted light cycles. Even when normal light–dark patterns were disturbed, consistent meal timing helped preserve some of the immune protection that would otherwise be lost.
This suggests that different circadian clocks in the body can compensate for one another. When the light-based clock is disrupted, food-related timing cues may help stabilize immune and metabolic rhythms. This insight has important implications, especially for environments where light exposure is difficult to control.
Why This Matters for Hospitalized Patients
The findings are particularly relevant for patients in hospitals, where circadian disruption is extremely common. Erratic lighting, nighttime clinical interventions, constant noise, and irregular meal schedules are routine in many hospital wards and intensive care units. For critically ill patients with respiratory viral infections, these disruptions may unintentionally worsen outcomes by interfering with circadian regulation of the immune system.
The CHOP researchers emphasize that circadian health is a modifiable factor. Unlike genetic risk or viral strain, environmental cues such as lighting and meal timing can be adjusted. The study calls for the integration of circadian-sensitive practices in clinical care. These could include structured light–dark cycles, minimizing unnecessary nighttime disturbances, and ensuring consistent meal timing whenever possible.
Such interventions are relatively low-cost and non-pharmacological, yet they may significantly improve immune function and accelerate recovery in patients with severe infections.
Broader Implications of Circadian Biology
Beyond influenza, circadian rhythms are known to influence responses to a wide range of diseases, including other viral infections, metabolic disorders, and inflammatory conditions. Immune cell trafficking, cytokine release, and tissue repair all follow circadian patterns. Disruption of these rhythms has been linked to worse outcomes in conditions ranging from sepsis to cardiovascular disease.
This field of research, often referred to as chronobiology, is increasingly shaping how scientists think about treatment timing. The concept of chronotherapy explores how aligning medical interventions with the body’s internal clock can improve efficacy and reduce side effects. While this study does not directly test timed medications, it strongly supports the idea that timing matters—not just for drugs, but for basic environmental conditions.
Practical Takeaways for Everyday Life
Although the study focused on preclinical models and hospital-relevant scenarios, the findings also offer lessons for daily life. Maintaining consistent sleep schedules, regular exposure to natural daylight, and predictable meal times may help support immune resilience. During periods of illness or recovery, protecting circadian rhythms could be an underappreciated component of healing.
As modern lifestyles increasingly disrupt natural biological rhythms, research like this highlights the importance of respecting the body’s internal timing systems. The immune system does not operate in isolation—it is deeply intertwined with the rhythms that govern nearly every aspect of physiology.
Looking Ahead
The CHOP study provides strong mechanistic evidence that circadian rhythms are not just background processes, but active determinants of infection outcomes. Future research may explore how these findings translate to human clinical trials and whether circadian-based interventions can measurably improve recovery in hospitalized patients.
As healthcare systems continue to search for ways to improve outcomes without relying solely on new drugs, circadian-informed care may represent a promising and largely untapped avenue.
Research paper reference:
https://www.jci.org/articles/view/193133