Junk Food Alters Brain Memory Circuits in Just Four Days, New Study Finds

Most people know junk food is not exactly good for the body, but recent research shows it can actually reprogram the brain’s memory center within days. A team of scientists at the University of North Carolina (UNC) School of Medicine has revealed that diets high in saturated fats quickly interfere with how brain cells process energy, leading to memory problems well before weight gain or diabetes ever show up.
This discovery, published in Neuron in September 2025, sheds light on why diet quality is directly tied to brain health and opens up new opportunities for interventions that could protect against long-term cognitive decline.
What the Study Showed
The researchers fed mice a short-term high-fat diet (stHFD) designed to mimic Western fast-food staples such as burgers and fries. Within just four days, the brain’s hippocampus—the region responsible for memory and learning—was noticeably affected.

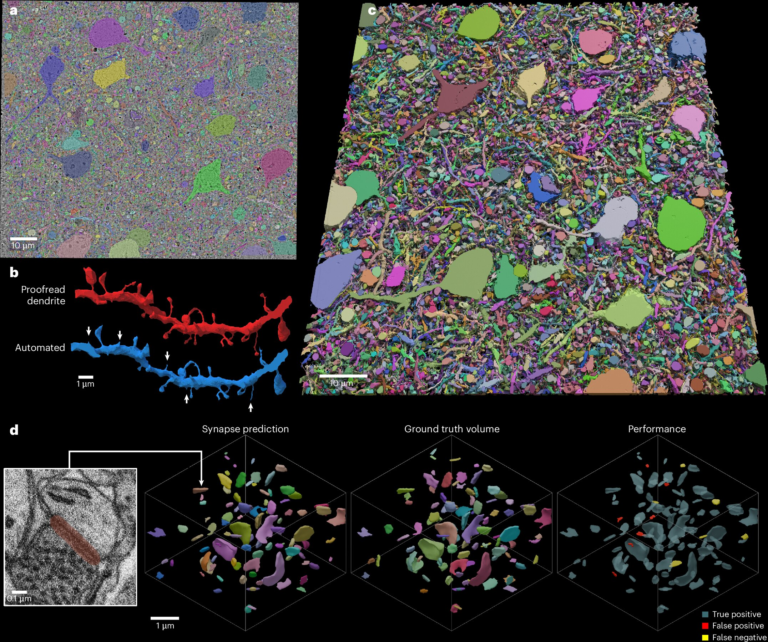
At the center of this disruption were CCK interneurons, a specialized group of cells in the hippocampus. These neurons became unusually active after exposure to the high-fat diet, and this hyperactivity was directly linked to reduced glucose availability in the brain. Since the brain depends heavily on glucose for energy, the lack of proper glucose intake meant that these neurons could not function normally.
This early dysfunction in memory-related circuits happened long before any visible signs of obesity or diabetes appeared, showing just how fast diet can affect the brain.
The Role of CCK Interneurons
The study specifically focused on cholecystokinin-expressing interneurons (CCK-INs) in the dentate gyrus region of the hippocampus. These neurons are glucose-inhibited, meaning their activity levels are strongly influenced by how much glucose is available in the brain.
When the brain’s glucose dropped due to the high-fat diet, these CCK-INs became hyperactive. This excessive activity disrupted normal hippocampal rhythms and impaired memory processing in the mice.
PKM2: The Molecular Link
The researchers also identified a key molecular player in this process: PKM2 (pyruvate kinase M2). This protein helps regulate how cells use energy through glycolysis. Under the high-fat diet, PKM2 activity increased, and this drove the hyperactivity of CCK interneurons.
When scientists either reduced PKM2 expression or inhibited its activity, the neurons calmed down and memory function improved. This finding is particularly important because it highlights PKM2 as a potential therapeutic target for protecting brain health in the context of poor diet or obesity.
Can the Damage Be Reversed?
One of the most promising parts of this research is that the harmful effects were not permanent.
When researchers restored glucose levels in the hippocampus, the hyperactive interneurons returned to normal activity, and the memory impairments disappeared. The team also showed that dietary modifications, such as periods of intermittent fasting following a high-fat diet, could normalize CCK interneuron activity and improve memory.
This means that early interventions—whether through food choices, fasting, or even pharmacological approaches—might help preserve memory function and reduce the long-term risk of neurodegenerative diseases like dementia and Alzheimer’s.
Why This Matters
The findings emphasize that the brain responds almost immediately to dietary influences. This has huge implications, especially in societies where high-fat junk food is widely consumed. If just four days of such a diet can disrupt memory circuits, then long-term habits could be far more damaging than previously thought.
By showing that memory decline can begin well before obesity or diabetes appear, the study also highlights the importance of preventive care. Addressing diet and metabolism early could lower the burden of age-related cognitive diseases.
Broader Implications for Alzheimer’s and Dementia
This research offers a new perspective on how metabolic disorders could contribute to neurodegeneration. Poor diet has long been associated with dementia risk, but the exact mechanisms were unclear. Now, with the identification of glucose-sensitive neurons and PKM2 activity, researchers have a clearer picture of how diet and brain function are connected.
Future studies will test whether these findings can be applied to humans. If they can, strategies such as dietary glucose stabilization, fasting regimens, or PKM2-targeted therapies might offer protection against cognitive decline.
Extra Information: Diet, Brain, and Memory
To give a fuller picture, here are some additional insights into how diet affects brain health.
The Brain’s Dependence on Glucose
The brain makes up only about 2% of body weight, but it consumes around 20% of the body’s glucose. Unlike muscles, which can switch to fat as an energy source, the brain depends heavily on glucose. When glucose processing is disrupted, even slightly, cognitive performance suffers.
This explains why conditions like hypoglycemia (low blood sugar) can cause confusion, memory lapses, and poor decision-making. The UNC study extends this knowledge by showing how a diet high in fat can indirectly reduce brain glucose availability, even when blood sugar levels are not drastically altered.
High-Fat Diets and Inflammation
Another well-documented effect of high-fat diets is increased inflammation. Chronic inflammation has been linked to both obesity and neurodegeneration. Inflammation in the brain can impair synaptic plasticity—the process that allows neurons to form and strengthen connections, which is critical for learning and memory.
The hyperactivity of CCK interneurons observed in the study could be part of this larger pattern of inflammatory and metabolic stress.
Junk Food and the Reward System
Junk food is engineered to be highly rewarding, often activating the brain’s dopamine pathways in ways similar to addictive substances. Over time, this can rewire the brain’s reward system, making it harder to resist unhealthy foods. When combined with the new evidence on hippocampal disruption, the picture becomes even more concerning: junk food may impair both decision-making and memory, creating a cycle that reinforces unhealthy eating habits.
Intermittent Fasting and Brain Benefits
The study’s mention of intermittent fasting is worth expanding on. Fasting has been shown in other research to improve insulin sensitivity, reduce inflammation, and promote autophagy, a process where cells clean out damaged components. All of these effects are believed to support brain health.
In the context of the UNC findings, fasting may also help restore glucose regulation in the hippocampus, preventing CCK interneuron hyperactivity and protecting memory.
PKM2 Beyond the Brain
PKM2, the enzyme highlighted in this study, is already known in cancer biology, where its altered activity helps tumors grow by shifting cellular energy metabolism. Now, its role in brain health adds another layer of importance. Targeting PKM2 may not only influence memory but could also have broader implications in treating diseases linked to abnormal metabolism.
Looking Ahead
The UNC team plans to continue studying how glucose-sensitive neurons disrupt brain rhythms that support memory. They also want to test whether their targeted therapies could be translated into human treatments.
The big takeaway is that what we eat doesn’t just affect our waistlines or blood sugar—it can quickly alter the very circuits of the brain responsible for memory. With dementia and Alzheimer’s cases on the rise, this research highlights an urgent need for more holistic health strategies that consider both body and brain.
Final Thoughts
This study is a powerful reminder that diet matters for brain health, and the effects can be surprisingly fast. While the research was done in mice, it points toward potential ways humans could protect memory through lifestyle changes and possibly new medical approaches.
The good news is that the damage isn’t set in stone—simple interventions like changing diet or fasting could help restore healthy brain function. For anyone worried about memory decline, paying attention to what’s on the plate might be one of the most important steps to take.
Research Reference: Targeting glucose-inhibited hippocampal CCK interneurons prevents cognitive impairment in diet-induced obesity