New Engineered Antibody Stops Cytomegalovirus From Evading the Human Immune System
Researchers at The University of Texas at Austin, working with international collaborators, have developed a newly engineered antibody that could significantly improve how the human immune system fights human cytomegalovirus (HCMV). This common but often overlooked virus infects a large majority of the global population and poses serious risks to newborns, transplant recipients, cancer patients, and people with weakened immune systems. The findings were published in Cell Reports (2025) and highlight a promising new direction for antiviral therapies.
Why Cytomegalovirus Is a Serious but Underestimated Threat
Human cytomegalovirus belongs to the herpesvirus family, which also includes viruses responsible for cold sores and chickenpox. Like its viral relatives, HCMV has the ability to remain in the body for life once someone is infected. For most healthy individuals, the virus stays dormant and causes no noticeable symptoms. However, the situation is very different for vulnerable populations.
HCMV is the leading infectious cause of congenital birth defects in the United States. It affects up to 2% of pregnancies worldwide, potentially leading to hearing loss, vision impairment, developmental delays, organ damage, and even death in newborns. According to estimates, over 80% of people globally are infected with the virus, making it one of the most widespread human pathogens.
Despite this prevalence and impact, there is currently no approved vaccine for HCMV. Treatment options are limited to antiviral drugs, many of which come with toxic side effects, can suppress bone marrow function, and often lead to drug resistance over time. These challenges have made it clear that safer and more effective therapies are urgently needed.
How HCMV Outsmarts the Immune System
One of the main reasons HCMV is so difficult to control is its ability to evade immune defenses. The virus has evolved sophisticated strategies to interfere with how antibodies normally work.
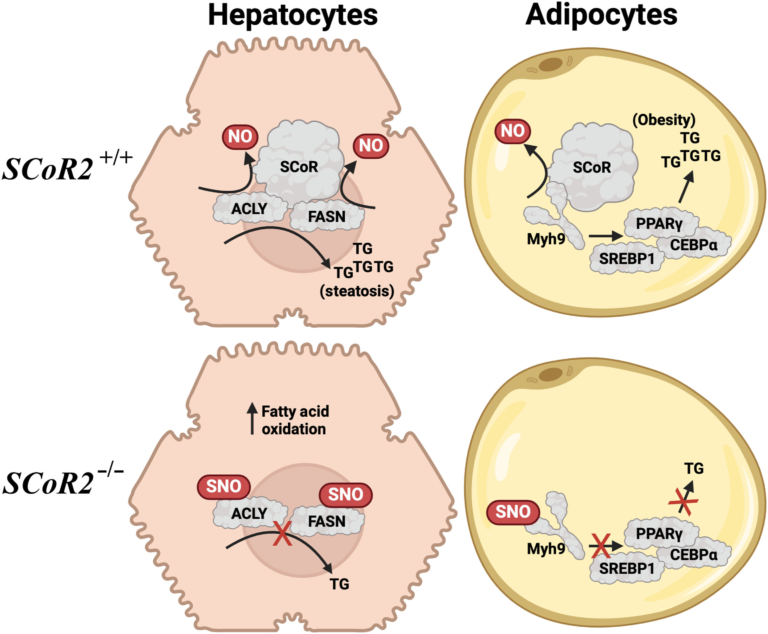
Under typical conditions, antibodies bind to viruses or infected cells and then recruit immune cells—such as natural killer (NK) cells—to destroy the threat. NK cells play a crucial role in clearing infected cells through a process known as antibody-dependent cellular cytotoxicity (ADCC).
HCMV disrupts this process by producing special proteins called viral Fc gamma receptors (vFcγRs). These viral proteins bind to the Fc region of antibodies, essentially hijacking them and preventing them from activating NK cells. As a result, infected cells are allowed to survive and continue spreading the virus.
This immune evasion mechanism is one of HCMV’s most effective survival tools and a major obstacle for antibody-based treatments.
The Breakthrough: Reengineering IgG1 Antibodies
The research team focused on a widely used and highly effective antibody type known as IgG1, which plays a central role in immune defense. By closely studying how HCMV interacts with IgG1 antibodies, the scientists identified the exact regions of the antibody that viral Fc receptors latch onto.
Using this information, they engineered a modified IgG1 antibody with subtle but critical structural changes. These changes prevent the viral Fc receptors from binding to the antibody while preserving its ability to interact with human immune receptors, including those on NK cells.
In simpler terms, the engineered antibody still activates the immune system but is no longer vulnerable to the virus’s tricks. This allows immune cells to recognize and destroy infected cells more effectively.
What the Experiments Showed
Laboratory experiments revealed several important outcomes:
- The engineered antibodies prevented HCMV from spreading between cells, a key feature that makes the virus so persistent.
- Viral dissemination was significantly reduced in infected cell cultures.
- NK cells regained their ability to recognize and kill infected cells when guided by the modified antibodies.
- The antibodies successfully avoided binding to viral Fc receptors while still engaging human Fc receptors, restoring normal immune function.
These results demonstrate that it is possible to selectively decouple viral immune evasion from immune activation—a major step forward in antiviral antibody design.
A Shift in How Antiviral Therapies Are Designed
Traditionally, antiviral treatments have focused on directly targeting the virus itself, either by blocking viral replication or neutralizing viral particles. This new approach takes a broader view by emphasizing the importance of empowering the immune system to eliminate infected cells.
Instead of just neutralizing free virus, the engineered antibodies help the body identify and clear infected cells, which is especially important for viruses like HCMV that hide within host tissues.
This strategy represents a paradigm shift in antiviral research. By targeting immune evasion mechanisms rather than the virus alone, therapies may become more durable, less prone to resistance, and better suited for long-term infections.
Who Could Benefit the Most
If future studies confirm these results in animal models and human trials, this approach could be particularly beneficial for:
- Organ transplant recipients, who often experience HCMV reactivation due to immunosuppression
- Cancer patients undergoing chemotherapy
- Newborns exposed to HCMV during pregnancy
- Individuals with inherited or acquired immune deficiencies
Because the engineered antibodies do not rely on toxic antiviral drugs, they may offer a safer alternative or complementary option for these high-risk groups.
Broader Implications Beyond Cytomegalovirus
The significance of this research extends beyond HCMV alone. Many other viruses—and even some bacteria—use similar strategies to interfere with antibody function. The antibody engineering techniques developed in this study could potentially be adapted to combat:
- Other herpesviruses
- Chronic viral infections with immune evasion mechanisms
- Certain bacterial pathogens that manipulate Fc receptor signaling
This opens the door to a new class of immune-focused therapeutics that could be applied across multiple infectious diseases.
What Comes Next
While the results are promising, the engineered antibodies are still in the early research phase. Several more rounds of testing are required before they can be considered for clinical use. The researchers are also exploring how this antibody design could be combined with:
- Existing antiviral drugs
- Future HCMV vaccines
- Other immune-based therapies
Such combination strategies could provide a more comprehensive and effective way to manage HCMV infection.
Why This Research Matters
HCMV has long been a neglected virus despite its massive global impact. This study highlights how a deeper understanding of immune biology can lead to innovative solutions that go beyond traditional drug development. By redesigning antibodies to outmaneuver viral defenses, scientists are showing that long-standing challenges in infectious disease treatment can be tackled in entirely new ways.
As research continues, this engineered antibody approach could mark an important step toward safer, smarter, and more effective antiviral therapies.
Research paper:
https://doi.org/10.1016/j.celrep.2025.116593