New Flu Research Shows Antibodies Can Do More Than Prevent Infection They Can Also Slow Transmission
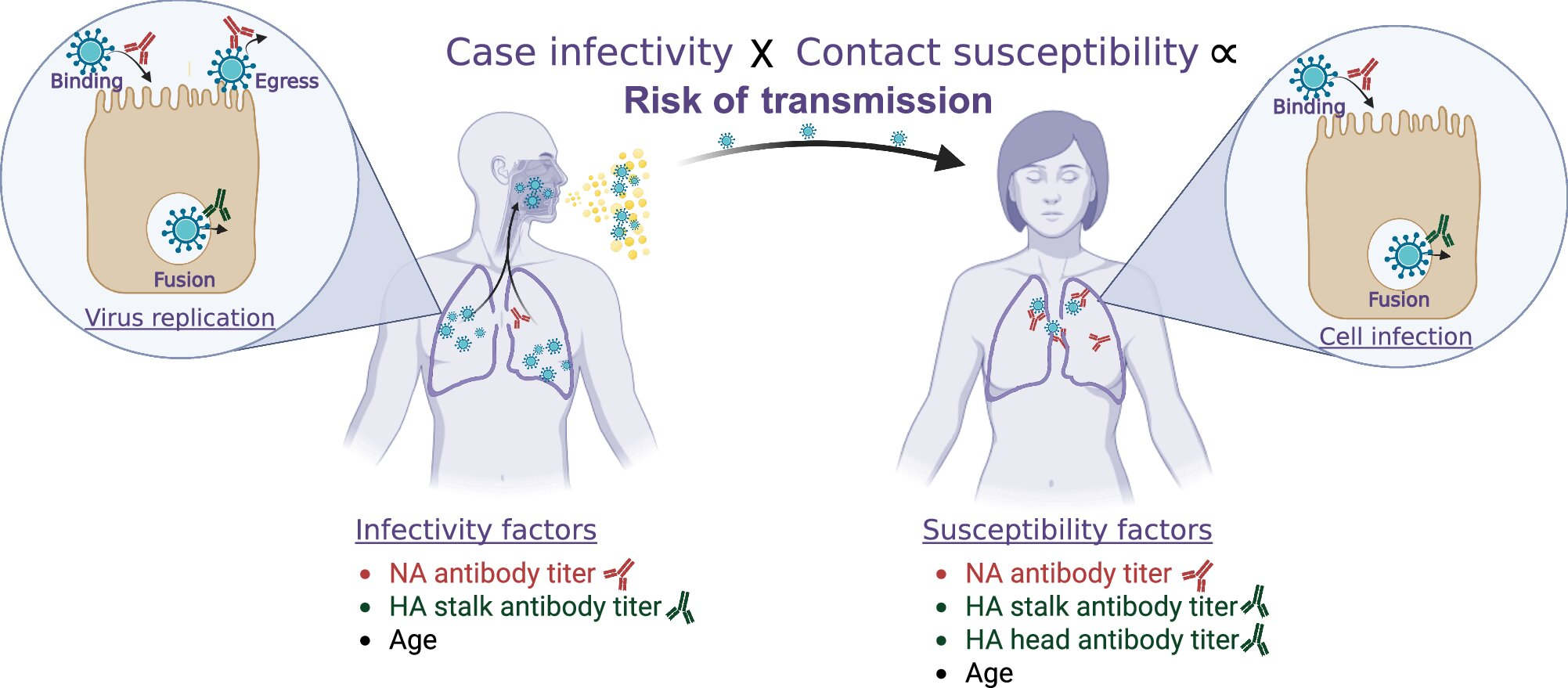
Influenza vaccines have long been designed with one main goal in mind: protecting individuals from getting sick. But new research published in Nature Communications suggests that flu immunity can do more than just prevent infection. Certain antibodies may also reduce how easily the virus spreads from person to person, opening the door to stronger and more community-focused flu vaccines in the future.
This large international study was led by researchers from the University of Michigan and Institut Pasteur, and it takes a closer look at how different types of influenza antibodies affect both susceptibility to infection and infectiousness once someone is sick. The findings arrive at a time when public health officials are warning about a potentially severe flu season and renewed concern over future influenza pandemics.
Why This Study Matters Right Now
Influenza remains a major global health problem. Each year, the flu infects more than 1 billion people worldwide and is responsible for around 650,000 deaths. Beyond the human cost, flu-related hospitalizations and lost productivity place a heavy economic burden on healthcare systems and societies.
Current seasonal flu vaccines are helpful, but their protection is often moderate and short-lived, usually lasting less than a year. By contrast, immunity gained after natural infection can protect against the same influenza strain for many years. Understanding why this happens — and how to replicate those benefits in vaccines — is a key goal of influenza research.
This new study helps bridge that gap by identifying which specific antibodies matter most, not just for preventing infection, but also for limiting transmission within households.
How the Research Was Conducted
The research team followed 171 households in Nicaragua, tracking a total of 664 participants across three influenza seasons: 2014, 2016, and 2017. This setting offered a unique opportunity because almost all participants were unvaccinated, allowing scientists to study immunity driven mainly by previous infections rather than vaccines.
The researchers combined several approaches:
- Blood samples to measure antibody levels
- Virologic testing to confirm influenza infections
- Detailed household monitoring to observe who infected whom
- Advanced mathematical modeling to estimate susceptibility and infectiousness
By analyzing these data together, the team was able to assess how pre-existing antibodies influenced both the likelihood of catching the flu and the likelihood of spreading it to others.
The Key Antibodies That Made a Difference
Influenza viruses have several surface proteins that the immune system can target. This study focused on antibodies directed against three major components:
Hemagglutinin (HA) Head
The HA head is the most familiar vaccine target. Antibodies against it were associated with a clear reduction in susceptibility, meaning people with higher levels were less likely to become infected. However, these antibodies showed little evidence of reducing infectiousness once someone was sick.
Hemagglutinin (HA) Stalk
The HA stalk is a more conserved part of the virus, meaning it changes less from year to year. Antibodies targeting the HA stalk were linked to both lower susceptibility and lower infectivity. In other words, people with these antibodies were less likely to get sick and less likely to pass the virus on.
Neuraminidase (NA)
Neuraminidase turned out to be especially important. Antibodies against NA were strongly associated with reduced susceptibility to infection and also reduced transmission risk. This finding is notable because NA has historically been underemphasized in flu vaccine design, despite being a key viral protein.
Together, the results show that not all antibodies are equal. Some play a dual role, protecting individuals while also lowering the chance that an infected person will spread influenza within their household.
Why Neuraminidase Has Been Overlooked
Most flu vaccines focus on hemagglutinin because antibodies against the HA head can block the virus from entering cells. However, the HA head mutates rapidly, which is one reason vaccine effectiveness varies so much from year to year.
Neuraminidase, on the other hand, helps the virus exit infected cells and spread to new ones. Antibodies against NA don’t always prevent infection entirely, but they can limit viral replication and reduce viral shedding, which directly affects how contagious a person becomes.
This study reinforces the idea that reducing transmission is just as important as preventing infection, especially in crowded households and communities.
Implications for Future Flu Vaccines
The findings suggest that future influenza vaccines could be improved by deliberately boosting antibodies against:
- Neuraminidase (NA)
- HA stalk
- HA head, as is already done
By targeting multiple viral components, vaccines could provide an extra layer of community protection, helping to shield people who cannot mount strong immune responses, such as infants, older adults, and immunocompromised individuals.
This approach could also be crucial during an influenza pandemic, when slowing transmission is just as important as protecting individuals from severe illness.
Why Studying Infection-Based Immunity Is So Valuable
Because so few participants in the study were vaccinated, researchers could observe how infection-induced immunity behaves in real-world conditions. This matters because infection often produces broader and more durable antibody responses than vaccination alone.
By identifying which antibody responses are most protective, scientists can translate these insights into better vaccine designs that aim for longer-lasting and more effective protection.
The Bigger Picture in Influenza Research
This study fits into a growing movement in influenza science that focuses on broadly protective and transmission-limiting immunity. Researchers around the world are exploring:
- Universal flu vaccines targeting conserved viral regions
- mRNA-based flu vaccines that include both HA and NA components
- Strategies that measure vaccine success not only by infection rates, but also by reduced spread
The idea is simple but powerful: a vaccine that slightly reduces symptoms but dramatically cuts transmission could still have a huge public health impact.
What This Research Ultimately Tells Us
The main takeaway is clear. Certain flu antibodies — especially those targeting neuraminidase and the HA stalk — play a critical role in both preventing infection and reducing contagiousness. This dual effect has been underappreciated in traditional vaccine strategies.
As influenza continues to evolve and pose seasonal and pandemic threats, studies like this offer valuable guidance on how vaccines can be redesigned to protect not just individuals, but entire communities.
Research Paper Reference:
https://www.nature.com/articles/s41467-025-65283-0