New Gene-Focused Approach Shows Promise for Treating Sepsis-Related Lung Injury
A new line of research is opening the door to potential treatments for one of the most dangerous complications of sepsis: acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). These conditions continue to carry high mortality rates, often around 40%, despite decades of supportive therapies like mechanical ventilation and antibiotics. A team led by Dr. YouYang Zhao at the Stanley Manne Children’s Research Institute, part of Ann & Robert H. Lurie Children’s Hospital of Chicago, has uncovered an unexpected biological mechanism that may finally offer a viable therapeutic direction.
The team’s work centers on a gene called ALOX15, which operates within the endothelium, the thin inner lining of blood vessels. While ALOX15 is known for producing certain bioactive lipids, its protective role in lung tissue under septic conditions had not been clearly defined until now. The group found that this gene—and the lipid signals it generates—may be essential for preventing severe lung damage during sepsis.
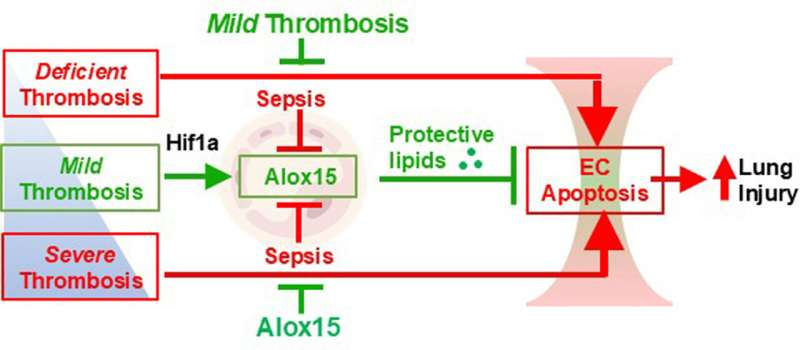
One of the most surprising findings emerged when the researchers studied the role of thrombosis, or blood clotting, in sepsis. Clinically, thrombosis is widely viewed as harmful during severe infections, and numerous trials of anticoagulant drugs have failed to show benefit for ALI or ARDS patients. But Dr. Zhao’s team discovered that although severe clotting does indeed worsen lung injury, mild clotting can do the opposite: it can actually protect lung tissue in mouse models of sepsis. This protective effect depends entirely on the activity of ALOX15.
Throughout the experiments, mice with mild lung thrombosis showed reduced injury severity, less endothelial damage, and better overall lung protection. When ALOX15 expression was high enough, this gene produced a specific protective lipid that helped maintain the stability of lung blood vessels. When ALOX15 expression was low, the mild clots no longer offered protection. This suggests that the quantity of ALOX15 activity—not just the presence of thrombosis—determines whether clotting is harmful or helpful. It introduces a new nuance into how scientists understand coagulation during sepsis.
The discovery is a major shift in conventional thinking. Traditionally, both “too much” and “too little” clotting have been considered universally detrimental in sepsis and ARDS. This research argues instead that the balance is what matters, and that ALOX15 is a central regulator of whether the lung vasculature can withstand septic injury. The researchers refer to this shift as a clarification of the extent to which clotting may actually act as a biological response meant to protect the lung—when supported by the right molecular environment.
Another crucial detail is that ALOX15 does not protect the lung by reducing clotting itself. Instead, the enzyme produces specific lipids that shield the endothelial cells from sepsis-induced damage. One of these lipids in particular was identified as a top therapeutic candidate in mouse studies. When administered to mice lacking ALOX15, the lipid significantly reduced lung damage, effectively substituting for the missing gene activity.
From a treatment standpoint, the study points to two promising strategies:
- Enhancing ALOX15 gene expression using an endothelium-targeted nanoparticle gene delivery system. Dr. Zhao has already developed and patented this technology.
- Developing treatments based on ALOX15-dependent protective lipids, which could potentially take the form of an oral medication.
If successful, these two strategies could create entirely new therapeutic avenues for sepsis-related lung injury—conditions that currently lack any targeted treatment. Unlike ventilation or antibiotics, which manage symptoms or infection rather than repairing damaged tissue, these approaches aim to protect and stabilize the lung’s vascular lining, addressing the core mechanism of injury.
The next step for Dr. Zhao’s team is to rigorously test the safety and effectiveness of both the gene-delivery approach and the lipid-based therapy in mouse models. These studies will help determine whether the findings could be translated into human clinical trials. If results are positive, early-phase trials could begin within two to three years, according to Dr. Zhao.
The research team brings substantial expertise to the table. Dr. Zhao serves as Director of the Genetic Medicine and Nanotechnology Development Center at Manne Research Institute and leads the Section for Injury Repair and Regeneration Research. He also holds the William G. Swartchild, Jr. Distinguished Research Professorship at Lurie Children’s and is a professor across Pediatric Critical Care, Pulmonary and Critical Care Medicine, and Pharmacology at Northwestern University Feinberg School of Medicine.
This work also highlights how much remains unknown about sepsis and ARDS, especially when it comes to endothelial behavior during widespread infection. Blood vessels are not passive conduits; they respond actively to inflammatory stress, and their dysfunction plays a key role in respiratory failure. Understanding how genes like ALOX15 govern endothelial resilience opens new scientific pathways that extend far beyond lung injury.
What Is Sepsis?
Since this topic often raises questions, it’s helpful to define what sepsis actually is. Sepsis is a life-threatening reaction to infection in which the body’s immune response becomes uncontrolled. Instead of fighting the infection efficiently, the immune system damages the body’s own tissues and organs, leading to shock and organ failure if untreated. The lungs are usually the first organ affected, which is why ARDS is so common in septic patients. As inflammation escalates, the blood vessels in the lung become leaky, oxygen exchange plummets, and the patient may require mechanical ventilation.
Understanding Acute Lung Injury and ARDS
Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS) represent two points on the same clinical spectrum. ALI is the earlier phase, marked by inflammation and fluid buildup in the lungs. ARDS is more severe and can require ventilatory support for days or weeks. Mortality increases with severity, with the highest risk in older adults and patients with pre-existing illnesses. Since there are no direct treatments that repair the underlying vascular damage, research into endothelial-protective mechanisms—like those driven by ALOX15—is crucial.
Why ALOX15 Matters Outside of Sepsis
ALOX15 is part of a family of lipoxygenase enzymes that help generate lipid mediators involved in inflammation and tissue repair. These mediators can both promote and resolve inflammation depending on the context. Previous studies have linked ALOX15 to:
- Vascular integrity
- Lung development
- Reducing oxidative stress
- Regulating immune cell responses
The gene’s specific role in protecting endothelial cells makes it a strong candidate for broader lung-health research beyond sepsis. Understanding how ALOX15 behaves in other diseases—such as pneumonia, viral ARDS, or even chronic lung conditions—may uncover additional therapeutic uses.
Why These Findings Are Different From Past Attempts
Attempts to use anticoagulant drugs in sepsis and ARDS have repeatedly failed, not because clotting is unimportant, but because clotting is not the root cause. By contrast, this study identifies a root-level protective mechanism tied to endothelial biology and gene-driven lipid production. Instead of suppressing a symptom (thrombosis), the research focuses on restoring the lung’s own built-in resilience system.
If these therapeutic strategies show success in humans, they could become the first targeted molecular treatments for sepsis-induced lung injury.
Research Paper:
Unexpected Protective Role of Thrombosis in Lung Injury via Endothelial Alox15