New Research Maps an Epilepsy Belt Across the United States Among Older Adults
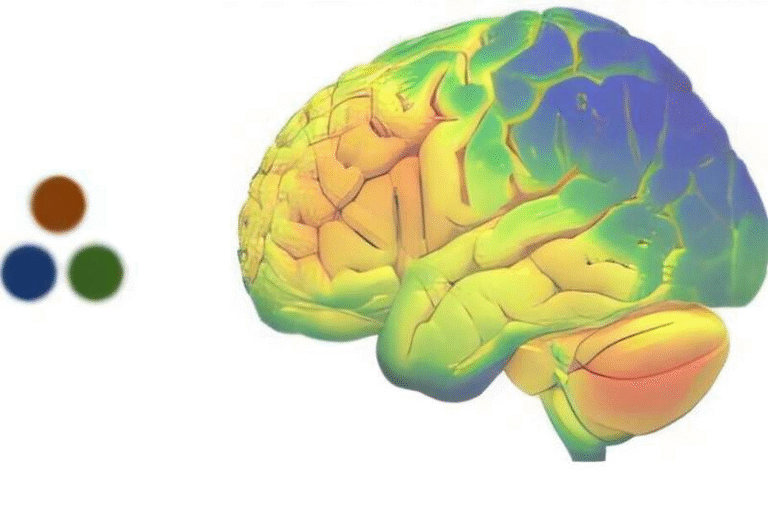
A major new national study has drawn a detailed map of epilepsy incidence among Americans aged 65 and older, revealing that some regions of the United States experience far higher rates than others.
The research—published in JAMA Neurology and conducted by teams from the Houston Methodist Research Institute and Case Western Reserve University—analyzed data from 4.8 million Medicare beneficiaries to identify where epilepsy strikes most often and what environmental and social factors may be driving those patterns. This is the first comprehensive attempt to chart epilepsy incidence among older adults at a nationwide level, providing clear geographic and contextual insights into a condition affecting an estimated 3.3 million people in the United States.
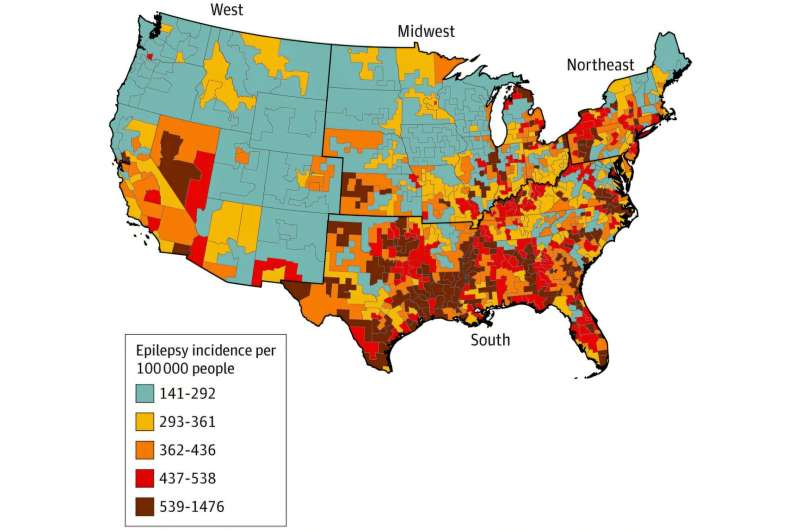
The study found significantly elevated epilepsy rates in parts of the South, especially Louisiana, Mississippi, East Texas, and central Oklahoma, compared with the rest of the country. These areas collectively form what researchers are now referring to as an epilepsy belt. According to the findings, the difference in incidence from one region to another was dramatic—more than a tenfold variation—with rates ranging from 141 to 1,476 cases per 100,000 people across the geographic units analyzed.
To generate these insights, researchers used advanced geospatial mapping and machine-learning methods applied to Medicare claims between 2016 and 2019. The dataset included oversampling of non-Hispanic Black and Hispanic beneficiaries to ensure more accurate representation of racial and ethnic groups. Alaska and Hawaii were excluded because their available data on social and environmental health indicators was incomplete. For geographic consistency and privacy protection, the research team aggregated U.S. counties into 692 “MaxCounties”, each with at least 11 identified epilepsy cases.
One of the most notable contributions of this study is its identification of several key factors strongly associated with increased epilepsy incidence among older adults. Among the most influential was insufficient sleep, defined as routinely getting fewer than seven hours per night in a given region. Areas where sleep deprivation was more common had almost twice the odds of high epilepsy incidence compared to areas with more adequate sleep levels. The role of extreme heat—measured through days with a heat index above 95 degrees—was also striking. This study is the first national analysis to reveal such a strong connection between high temperatures and new epilepsy diagnoses in older adults. With the ongoing impacts of climate change and a rapidly aging population, this link suggests potential future challenges for public health planning.
Additional factors associated with higher epilepsy rates included low physical activity, higher obesity prevalence, limited access to primary care physicians, and lack of access to household vehicles. In fact, insufficient vehicle access showed an association nearly equal to that of insufficient sleep, indicating that basic transportation availability may play a crucial role in whether individuals can seek timely medical evaluation or manage existing health issues. Another notable association was the higher incidence of epilepsy in areas where younger adults lacked health insurance, which researchers believe may point to delayed diagnoses that only surface once individuals become eligible for Medicare at age 65.
All these variables fall under the umbrella of social and environmental determinants of health, reinforcing the idea that epilepsy risk is not solely a biological matter but is strongly influenced by living conditions, community infrastructure, and environmental stressors.
The mapping itself yielded patterns that were previously invisible when looking at national data in a more generalized way. By analyzing neighborhood-level indicators such as sleep habits, heat exposure, and healthcare access, the researchers uncovered a clearer picture of how these factors combine in identifiable geographic clusters. This nuanced approach allows for a better understanding of where targeted interventions could be most effective.
The economic weight of epilepsy on the U.S. healthcare system underscores the importance of such research. In 2019, spending related to epilepsy and seizure disorders reached $24.5 billion, emphasizing the need for strategies that not only treat epilepsy but help reduce incidence through preventive measures. By identifying where the burden is greatest, policymakers and health systems can begin to allocate resources more effectively and develop region-specific plans for reducing risk.
One broader contextual point is that this newly defined epilepsy belt overlaps partially with the well-known Stroke Belt, another region where neurological conditions occur at elevated rates. While the causes are not identical, shared environmental and socioeconomic factors may influence both patterns. Understanding these overlaps may help researchers pinpoint deeper structural contributors to neurological disease risk.
Because this study focuses specifically on older adults, it also raises important questions about the aging population in the United States. Older adults have a higher baseline risk for epilepsy compared to younger adults, often due to strokes, neurodegenerative conditions, and other chronic diseases. This new research suggests that where older adults live—and the environmental pressures they face—may be just as important as their personal medical history.
Below are some additional insights that provide useful background for readers learning about epilepsy and why studies like this matter.
What Epilepsy Is and Why Older Adults Are at Higher Risk
Epilepsy is a neurological condition characterized by recurrent, unprovoked seizures. While often associated with childhood, epilepsy actually has a second peak later in life. Among adults over 65, risk factors include strokes, brain injuries, tumors, neurodegenerative disorders like Alzheimer’s disease, and long-term vascular problems. Since the U.S. population is aging, understanding how and where epilepsy develops is an essential part of preparing the healthcare system for shifting demographics.
How Environmental and Social Conditions Influence Neurological Health
Environmental stressors and social conditions can influence the brain in ways that increase susceptibility to seizures. Extreme heat, for instance, can affect cardiovascular function, hydration, and stress hormones—all of which can influence neurological stability. Sleep deprivation reduces the brain’s threshold for electrical disturbances, making seizures more likely. Low physical activity can contribute to poorer metabolic and vascular health, both of which are associated with neurological conditions. Limited transportation access may lead to delayed diagnosis or poor management of chronic health issues, indirectly increasing epilepsy risk.
Why Mapping Disease Incidence Matters
Geospatial health research—like the approach used in this study—helps reveal clusters and patterns that normal health data might overlook. When a disease disproportionately affects certain regions, it suggests that localized factors are at play. This knowledge allows policymakers to create region-focused interventions, such as improving healthcare access, offering community-based health education programs, or implementing climate-related resilience strategies for vulnerable populations.
Mapping also helps communities understand their own health risks. Identifying an epilepsy belt provides an opportunity for states within that region to collaborate on prevention and early detection strategies.
What Future Research Can Build On
While the study identifies strong associations, it does not establish direct causation between environmental factors and epilepsy. Future research could explore how climate, socioeconomic factors, and healthcare access individually and collectively influence epilepsy risk. This may eventually lead to more precise public health recommendations or early-warning systems in high-risk areas.
Research Source
Incidence and Risk Factors of Epilepsy Among Older Adults in the US Medicare Population (JAMA Neurology, 2025)
https://doi.org/10.1001/jamaneurol.2025.4347